Holiday Greetings from Professor Mignon McCulloch, President of IPTA
Dear All
It is my privilege to be the President of a professional organization which has as our goal the advancement of science and practice to improve the health of children who require transplantation in the worldwide community, and to advocate for their rights.
As 2019 draws to a close and we enter the Holiday season, it is a good time to reflect on what we have achieved this year. The highlight has been the very successful IPTA 2019 Congress in Vancouver hosted by Anne Dipchand as President, with over 500 delegates, which was a wonderful opportunity for sharing of knowledge and networking with friends and colleagues.
The Scientific Advisory Committee (SAC) produced an excellent academic content under Catherin Parker’s wise guidance with the Local Organising Committee under Tom Blydt-Hansen. Amongst their other duties, they also produced spectacular weather in Vancouver for the duration of the meeting. A special thanks to Isabel Stengler and her team for ‘making it all happen’ and to Sondra Livingston, Robert Colarusso, and the rest of the TTS team for all of their efforts in making this a successful meeting.
Our journal Pediatric Transplantation has also had a successful year under the leadership of our new editors Burkhard Tönshoff and Sharon Bartosh. Since this meeting, our IPTA Council has had some new members rotate onto the Council to join our wise group to ensure collective international input. I am grateful to those who have rotated off and know that they have been available for ongoing input when needed, and I am also excited about the new members and the talents that they bring to the organisation.
The various IPTA sub-committees have been hard at work with new goals and objectives, amongst the highlights including:
- Education Committee facilitating the first TTS-IPTA joint webinar on Epitope Matching;
- Ethics committee producing thought provoking case discussions and planning ethics-related position statements;
- Outreach committee relaunching their program and developing a collaborative program between Dallas, USA and Bangalore, India, launching in 2020 and exploring multi-lingual patient education resources;
- Membership committee developing new initiatives to increase membership and planning new opportunities for enhanced engagement of members including senior and junior members interaction;
- Allied Health committee providing an excellent pre-congress symposium at the IPTA 2019 meeting together with large numbers of Allied Health colleagues also attending the main congress, developing a survey and planning webinars in the future;
- Publications committee producing our informative newsletters, planned development of a peer mentoring program, and collaboration with the editors of Pediatric Transplantation;
- Infectious Disease committee continuing to be prolific in their aims to spread knowledge about ID in pediatric transplantation with a successful EBV consensus meeting, a number of publications including a PJP survey, Live virus vaccines as well as collaboration with IPTA colleagues across the globe;
- We would also take this opportunity to welcome our newest committee, the Communications committee, who are responsible for developing our social media communications as well as the optimization of a newer IPTA Website.
I would like to thank the IPTA Council as well as the Committees and their respective chairs for being so active and providing valuable input into our organization.
We look forward to our next IPTA congress, 17 – 21 April 2021 in Prague, and thank Lars Pape and George Mazariegos, together with Catherin and Isabel from TTS, who are already hard at work with the SAC in planning this meeting, as well as our local host, Tomas Seeman.
Finally I would like to thank the Executive Committee with Anne Dipchand (Past President) as a wise counsel, Carlos Esquivel (President Elect) for his enthusiasm and support and Lars Pape (Secretary/Treasurer) for his fresh ideas and treasurer input over this year.
I would also like to thank Katie Tait from TTS for her significant administrative support and never-ending cheerfulness.
On behalf of this group, I would like to wish all our members a Happy Holiday season hoping that you do get some ‘time-out’, and especially wishing you special time with your loved ones.
Thank you for all you do in your daily capacity to improve the health of all the pediatric patients in your care, and furthering the mission of our society.
May you all have an exciting start for 2020!
Best wishes
Mignon McCulloch
IPTA President
TTS 2020
We are delighted to confirm that IPTA will have a presence at the 28th International Congress of The Transplantation Society, September 12-16 2020, in Seoul, South Korea.
Our programming will include a pre-Congress session on September 13th from 8am-3pm, 1 SOTA, 1 EMW, and abstract sessions. Please watch out for abstract submission deadlines. We will publish more information on this event closer to the time.

This newsletter’s literary highlights come from Katherine Twombley, Chief, Pediatric Nephrology Interim Chief, Pediatric Neurology, Medical Director, Pediatric Kidney Transplant, Medical Director, Acute Dialysis Units, Medical University of South Carolina
With a shortage of organs in the United States, many people are looking at way to increase decreased donor donation. In a recent article published in Pediatric Transplantation entitled “Crowdsourced analysis of factors and misconceptions associated with parental willingness to donate their child's organs,” Jones et al. took on this very tough but extremely important topic. They evaluated factors associated with parent’s willingness to donate their child’s organs. They sent out surveys using Amazon's Mechanical Turk (MTurk) Prime platform. They targeted 400 respondents and received 425.
Similar to previously reported data, about three quarters of respondents would consider donating their own organs, but only about 65% were actually willing to donate their child’s organs. Unfortunately, less than half of the respondents believed that declaring someone brain dead means that they are dead and lower income respondents were more likely to have this belief.
Black respondents were 5.3 times more likely compared to White respondents and Hispanic respondents were 2.24 times more likely compared to White respondents to think that doctors are “stealing” organs from patients. Black (4.97 times) and Hispanic (2.18 times) respondents were also more likely than White respondents to believe that doctors are declaring patients brain dead based on their skin color or how much money they have. The odds of continuing to have this belief decreased as income increased.
This study highlights the persistent mistrust that some racial and ethnic groups have toward doctors. These beliefs are deeply rooted in past mistreatments as the authors point out (Tuskegee syphilis experiment, Tucker’s Heart, etc.), and we as a community need to make every effort to not only understand these perceptions, but also work hard to address and educate patients about these beliefs.
With the growing use of internet and social media, comes a plethora of misinformation. It is sometimes hard for families to know what information is fake. Interestingly, respondents that had a family member declared brain dead in the past were more likely to donate organs. This really emphasizes the value of what good communication and education with families can do. Future studies will need to look at the best methods of education and communication with families of different socioeconomical and racial backgrounds to improve the relationships we as doctors have with our patients.
Ethics Case: Minors as living donors
Glenda Moonsamy
Charlotte Maxeke Johannesburg Academic Hospital, Department of Paediatrics and Child Health
University of the Witwatersrand, Faculty of Health Sciences
Johannesburg, South Africa
Case study:
A female baby was born to teenage parents with bilateral multicystic dysplastic kidneys and renal failure. Her family was counselled with respect to her condition and poor prognosis immediately after birth. Both her parents were scholars. Her mum was 16 and dad was 17 years old respectively. However, both parents had supportive extended families even though their socio-economic status was poor. The parents had also ended their relationship prior to the birth of the baby. The mum and her family were the primary caregivers.
Despite her renal failure, the baby thrived and at the age of 6 months, after careful consideration, it was decided that she be initiated onto peritoneal dialysis. The year post dialysis was difficult, with the child developing multiple bouts of peritonitis and having a short period of intermittent hemodialysis. She eventually settled on peritoneal dialysis and reached a weight suitable for dialysis at 2 years of age. During this period, despite the mum attending school full time, she and her family were very compliant, responsible and demonstrated unwavering support for their little girl. The parents were again counselled with respect to transplantation and being potential related living donors, to which they both agreed. In Johannesburg, the donor age requirement is 21 years.
Her case was presented to the renal transplant panel and after some deliberation, she was accepted for both a related living donor and cadaver transplant. Her dad was a blood group match and was worked up as a potential donor. He was 19 years old at the time and again, was still in school. However, during this period a cadaver donor became available and our patient was successfully transplanted.
Ethics comment:
In an era where the demand for organs outweighs the supply, careful consideration of the potential for expanding the related living donor pool has to be taken into account. Using minors as donors is a possible but controversial solution. The KDIGO guidelines accept an age requirement of 18 years. But at 18 years (or even 21 years for that matter) are you mature enough to give an informed consent, identify the risks to yourself and decide on your moral obligation? The risks to benefit need to be carefully weighed in each individual case.
There are many variables contributing to the development of life skills and maturity, including life experience, personality, morals, values and even genetics. This makes an age criteria difficult. However, it is a necessary requirement in our circumstances when considering a potential living donor. It should be taken into account together with the other pre-requisites like psychological and social functioning to determine whether the minor is a mature minor with the appropriate level of neurocognitive and emotional development.
With respect to the case above, the situation is a bit unique, but does an unplanned teenage pregnancy award you such insight and maturity, despite being an emancipated minor? The birth of a child is certainly a life changing experience, and in this scenario, it was compounded by a baby with chronic kidney disease. The family’s investment into the baby’s care helped in assessing the situation but it did not make the decision to initiate dialysis or use the parents as related living donors any easier.
UPDATE FROM THE OUTREACH COMMITTEE

Dear IPTA Colleagues,
The Outreach Committee is pleased to announce that applications for the 2020 Outreach Program are open. The program supports emerging centres that seek to develop or expand/enhance care in existing transplant programs.
Usually, an emerging centre will have identified a suitable supporting centre to assist them with this program; however it is possible the Outreach Committee can assist in this process.
The application package, guidelines and useful reference documents are available on the Outreach Program section of the IPTA website.
Application Deadline: February 28th, 2020
With many thanks,
Fiona Mackie
Chair, Outreach Committee
UPDATE FROM THE MEMBERSHIP COMMITTEE

Dear IPTA Colleagues,
The Membership Committee is interested in creating a database of expertise among our members, with the goal of highlighting the breadth of our membership and also utilizing the database as a resource for members looking to connect with others in their area for mentorship, collaboration, etc. We are also interested in gaining a better understanding of the diversity of languages spoken among our membership for future educational opportunities. Please email Katie Tait, This email address is being protected from spambots. You need JavaScript enabled to view it., with the following information:
- Areas of expertise
- Languages spoken
- Are you interested in being approached to participate in future educational opportunities or to be contacted by members from other centres?
Many thanks for your support,
Cozumel Pruette
Chair, Membership Committee
EXCITING NEWS FROM ID COMMITTEE
Dear IPTA Colleagues,
The IPTA IDCARE committee has completed initiatives related to:
how to approach SOT candidates with active infections (https://www.ncbi.nlm.nih.gov/pubmed/30838753), review of recent CMV guidelines with pediatric-specific cases (https://onlinelibrary.wiley.com/doi/full/10.1111/petr.13276), and emerging mosquito-borne viruses and impact on transplant (https://www.ncbi.nlm.nih.gov/pubmed/30338634). Committee members have actively participated in consensus meetings related to the diagnosis, management, and prevention of EBV-associated PTLD, as well as an evidence review of live-attenuated virus vaccination in selected SOT recipients, with expert recommendations recently published (https://onlinelibrary.wiley.com/doi/full/10.1111/petr.13571). The IDCARE committee continues to work on various infectious disease topics including providing updates on influenza – infection and vaccination for this season, summarizing a multidisciplinary approach to the evaluation of diarrhea in solid organ transplantation recipients, assessing prophylaxis strategies for PCP and toxoplasmosis across pediatric SOT centers, reviewing infectious complications of asplenia, including optimizing prevention strategies, and summarizing the results of a survey regarding contemporary practice for live-attenuated vaccination in solid organ candidates and recipients. The IDCARE committee continues to welcome IPTA members to provide feedback for topics of interest and potential collaborative projects.
Many thanks,
Monica Ardura
Chair, ID Committee

IPTA READERSHIP SURVEY
FOR READERS OF PEDIATRIC TRANSPLANTATION
Pediatric Transplantation is the official journal of IPTA. At the link below, you will find a survey created by the IPTA Publication Committee and IPTA Leadership regarding the journal. We hope to continue to improve the services the journal provides to you, our members. This survey will help us identify areas to expand or improve. We promise it will not take more than a few minutes to fill out.
TTS ANNOUNCEMENTS

On behalf of IPTA, we wish you a happy holiday season, with our best wishes for 2020!
Past Issues


Message from IPTA President
Dear All,
I am really delighted to be part of this enthusiastic and active IPTA community and would like to thank Anette Melk and the Publications committee for putting this newsletter together, showcasing just some of the exciting projects that IPTA has been developing.
I would urge you all to Save the Date for IPTA 2021 in Prague.
Best wishes,
Mignon McCulloch
IPTA President

This newsletter’s literary highlights come from Lars Pape, Univ. Prof. Dr. Med., Hannover Medical School, MHH – Clinic for Paediatric Nephrology, Hepatology and Metabolic Disorders.
- R. J. Arasaratnam, I. Tzannou, T. Gray, P. I. Aguayo‐Hiraldo, M. Kuvalekar, S. Naik, A. Gaikwad, H. Liu, T. Miloh, J. F. Vera, R. W. Himes, F. M. Munoz, A. M. Leen
Dynamics of virus‐specific T cell immunity in pediatric liver transplant recipients. Am J Transplant 2019; 18(9): online first.In this manuscript the authors describe the clinical course of EBV, CMV, HHV6 and BKPyV specific T cells in children after pediatric liver transplantation. This manuscript is the first to prove in children after liver Tx that Virus specific T cells can be a useful tool in monitoring the cellular immune response to different viral disease dependent on change of immunosuppression and implementation of antiviral therapy. Future interventional trials will have to prove the additional value of this monitoring tool for infection control and graft survival.
- Bonthuis M, Groothoff JW, Ariceta G, Baiko S, Battelino N, Bjerre A, Cransberg K, Kolvek G, Maxwell H, Miteva P, Molchanova MS, Neuhaus TJ, Pape L, Reusz G, Rousset-Rouviere C, Sandes AR, Topaloglu R, Dyck MV, Ylinen E, Zagozdzon I, Jager KJ, Harambat J.
Growth Patterns After Kidney Transplantation in European Children Over the Past 25 Years: An ESPN/ERA-EDTA Registry Study. Transplantation 2019 Apr 1.This manuscript shows in more than 3400 European pediatric kidney recipients differences in growth patterns linked to the country they come from. Only a little more than half of the children have normal height SDS values. Especially the youngest children hat the most severe growth retardation and growth hormone was not routinely used in many patients of this cohort. Additionally, no follow-up growth could be determined in children transplanted above an age of 12 years. This paper is therefore an important contribution that should enforce all of us in early use of adequate nutrition and growth hormone in chronic renal failure in order to improve final height of children before and after kidney transplantation.
- Yevgeniya Atiskova, Simon Dulz, Kaja Schmäschke, Jun Oh, Enke Grabhorn, Markus J. Kemper, Florian Brinkert
Oxalate retinopathy is irreversible despite early combined liver‐kidney transplantation in primary hyperoxaluria type 1. Am J Transplant 2019; (18)9: online first.This manuscript evaluated the course of oxalate retinopathy in children before and after combined pediatric Liver and Kidney Transplantation. The authors could show that time to transplantation was associated with worse oxalate retinopathy and that no improvement of oxalate deposition could be found after transplantation. Therefore, this paper underlines the need for early diagnosis of Hyperoxaluria combined with early interventions as Vitamin B6 therapy, combined peritoneal- and hemodialysis, combined Liver- / Kidney Transplantation as well as new emerging therapies as Oxalobacter perfringens or gene therapeutics in order to inhibit the development of systemic oxalosis as much as possible.

Dear IPTA Colleagues,
Would you like help from senior members to refine your research question or review your manuscripts to increase likelihood of publication? The Publications and Communications Committee would like to invite you to participate in the Peer Mentoring designed to increase access to experienced reviews. We would like to offer to participants a chance to have a dialogue with those experienced in the publication process prior to final submission. Responsibilities of your mentor would include reviewer style feedback to the mentee and availability for subsequent questions. Mentors would also be available to refine language to meet standards for publication, especially for non-native English speakers. We are also looking for suggestions of names of others who might be interested and encourage junior faculty and allied health members to join!
If you are interested, please send your name, email, and any specific areas of research focus to This email address is being protected from spambots. You need JavaScript enabled to view it..
Thank you in advance for your support,
Peer Mentoring Workgroup, IPTA
Chesney Castleberry, Workgroup Leader, IPTA Publications Committee

Dear IPTA Colleagues,
The Allied Health (AH) held its first all day pre-congress symposium entitled ‘Improving Outcomes in Pediatric Transplant: A Collaborative and Comprehensive Approach to Care’. It was a great success with over 60 attendees from 8 different countries in attendance including nurses, social workers, psychologists, pharmacists, occupational therapists, physiotherapists, dietitians, transplant coordinators, chaplains, students and researchers from various disciplines! The symposium included amazing speakers and panel discussions covering a broad range of topics including:
- The Family in Stress: Assessment, strategies and outcomes
- Avatars for Adherence? Utilizing the digital world to improve outcomes
- Back to Basics: Talking instead of texting
- Social Media: Friend or foe (debate)
- Sex, Drugs, Rock 'n roll: Lifestyle guidelines
- The Role of Palliative Care in Paediatric Transplantation: A panel discussion
Please log in to the congress website to see recordings of the sessions!
In addition, over 70 Allied Health delegates registered for the congress. From Allied Health, there were 6 abstracts presentations, 8 mini-abstract presentations, 11 posters presentations and interactive workshops on the following topics:
- Nutrition and Oral Feeding
- Frailty as a Concept in Pediatric Transplantation
- Interventions and Outcomes in Transition: Engaging Adolescents in the Transition Process
- Ethical Issues in Pediatric Transplantation: When a Patient is No Longer a Transplant Candidate
Finally, we also hosted an open Allied Health Professionals business meeting, followed by a social event, which provided a great opportunity to meet new colleagues, network and share ideas.
IPTA, TTS and CST Scientific Awards Winners
Congratulations to all the AH professionals whose great work and positive contributions to the organization were recognized through awards:
- Beverly Kosmach-Park was awarded the Distinguished Allied Health Professional Award
- Research awards were given for the following projects:
- Anna Gold - Early School Age Cognitive Performance Post Pediatric Heart Transplantation
- Catherine Patterson - Neurodevelopmental Motor Outcomes in Young Children Pre and Post Liver Transplant
- Taylor Melanson - Prevalence and Consequences of Medication Non Adherence in Pediatric Kidney Transplant Recipients in the United States 2005-2015
- Jenny Velasco - Overweight and Obesity Prevalence in Children After Transplant: Short and Medium Term Evolution
- Robin Deliva - Neurodevelopmental Outcomes in Young Heart transplant recipients
- Mar Miserachs - Standardized Feeding Protocol Following Pediatric Liver Transplantation – A Pathway for Improved Nutritional Care
AHP Committee Initiatives for 2019-2021
- Allied Health Membership and Focus Survey
To describe the prevalence, diversity and clinical practice focus of AH team members within each centre globally. This information will serve as a foundation to help inform and develop a greater understanding of multi-disciplinary team composition, and frameworks regarding professional practice. Watch your inbox for a survey coming later 2019! - Maintain regular communication with Allied Health
To continually update the Allied Health Professional page on the IPTA website including regular profiling of AH members, update of committee initiatives and membership benefits. Check out our webpage for upcoming features including ‘Get To Know Your AH Colleagues’, with member profiles every two months and updates on AH related research projects. - Continuing education with AH members through the development of a series of webinars
To develop a series of webinars covering a range of relevant AH topics and drawing upon the expertise of members. The topics for these webinars will be informed by the AH survey results and direct feedback from our members during the IPTA 2019 Congress. Stay tuned!
Upcoming Goals for IPTA 2021 Congress (Prague, Czech Republic)
Plenary and State-of-the Art presentations on AH topics is currently in the planning phase! Be sure to save the date for Prague 2021!
Many thanks for your support,
Anna Gold and Jenny Wichart
Co-Chairs – IPTA Allied Health Professional Committee

Please find this update on Pediatric Transplantation from the Editors-in-Chief Sharon Bartosh and Burkhard Tönshoff.
The Author Guidelines for Pediatric Transplantation have recently been revised (click here). There you will also find the respective links to a number of Research Reporting Guidelines such as CONSORT for randomized trials, STROBE for observational studies, PRISMA for systematic reviews and CARE for case reports, beside others. Accurate and complete reporting enables readers to fully appraise research, replicate it, and use it. Authors are encouraged to adhere to recognized research reporting standards. The EQUATOR Network has collected more than 370 reporting guidelines for many study types (click here to visit the website).
Pediatric Transplantation offers the publication of Special Issues such as a series of articles derived from a consensus conference, with all review articles on a particular topic published in one issue. If you plan such a conference, consider to publish the consensus document and/or the respective review articles in our journal. Please contact the Editors-in-Chief Sharon Bartosh and Burkhard Tönshoff beforehand (This email address is being protected from spambots. You need JavaScript enabled to view it., This email address is being protected from spambots. You need JavaScript enabled to view it.).
IPTA Readership Survey for readers of Pediatric Transplantation>
Pediatric Transplantation is the official journal of IPTA. At the link below, you will find a survey created by the IPTA Publication Committee and IPTA Leadership regarding the journal. We hope to continue to improve the services the journal provides to you, our members. This survey will help us identify areas to expand or improve. We promise it will not take more than a few minutes to fill out.
IPTA Publication Committee and IPTA Leadership


Message from Dr. Mignon McCulloch
Dear IPTA members and attendees of the IPTA 2019 Congress,
We would like to thank you for your part in attending and participating to make the IPTA 2019 Vancouver Congress such a hugely successful Congress and opportunity to network with friends and colleagues in the beautiful city of Vancouver. Learning in such a beautiful environment was not a hardship.
If you didn’t get the chance to join this time around, we hope that you can join us in Prague in 2021. Furthermore, if you are a member of IPTA, you can access the recordings via our section website. You are able to watch the talks and presentations HERE (member login required).
We would like to share with you some of the interesting facts from this meeting
- We welcomed 522 participants from 36 countries.
- The Congress started with a special opening address and blessing by Elder Roberta Price.
- Totem poles watched over speakers as they shared knowledge with friends and colleagues.
- Pre-meeting symposia including a Writing Course workshop, Foundations in Pediatric Transplantation “long-term outcomes” and a first-ever all-day Allied Health Symposium on Improving Outcomes in Pediatric Transplantation took place on May 4.
- We remain very grateful for generous sponsorship from UPMC Children’s Hospital of Pittsburgh, Astellas, One Lambda, Stanford Children’ Health & Lucile Packard Children’s Hospital Stanford, Dr. Ken Citron Charitable Trust and Bryce Cormier Memorial Fund as well as all our many collaborating hospitals & non-profit organizations.
PROGRAM HIGHLIGHTS AT A GLANCE
- 323 abstract submissions from 34 countries
- 115 invited speakers from 13 countries
- 6 Plenary Symposia
- 5 State-of-the Art Presentations
- 3 Pre-Congress Symposia
- 16 Interactive Workshops
- 21 Oral Abstract Sessions
- 3 Poster Sessions and
- 2 Morning Industry Symposia
- Abstracts were published in Pediatric Transplantation Journal
We look forward to welcoming you to the next IPTA Congress in Prague, Czech Republic. Please mark your calendars: April 17-20, 2021.

Until then… please remain involved in our organization by looking out for our newsletters, joining us as a member, and visiting our website.
Best wishes,
Mignon McCulloch
IPTA President and IPTA 2019 Co-Chair
Carlos Esquivel
IPTA President-elect and IPTA 2019 Co-Chair


Message from Dr. Anne I. Dipchand
Dear Colleagues,
It is hard to believe that it has been 2 years since we all saw each other at IPTA 2017 in Barcelona! It has been a very productive two years for IPTA. The last two years saw significant change to the organization starting with a move to a new management company under the umbrella of TTS while maintaining our status as an independent association. This has been an excellent move for IPTA, has strengthened us financially, and opened the door for many more collaborations with TTS and other professional transplant organizations. Our Journal saw a transition to new editors, Burkhard Tonshoff and Sharon Bartosh, who have been busy implementing new initiatives to enhance Pediatric Transplantation.
Our committees have been very active in the last 2 years. The IPTA ID CARE Committee has continued to be very prolific, hosting a live vaccine consensus meeting, updating the pediatric CMV guidelines, co-hosting an EBV/PTLD symposium, amongst other clinical academic pursuits which will guide our practices for the foreseeable future. The IPTA Allied Health Committee has contributed significantly to programming for IPTA 2019 including a full day pre-symposium in addition to surveying Allied Health colleagues widely in order to determine how best to provide for this important part of IPTA membership. The IPTA Education Committee has continued providing educational programming to multiple meetings including the successful IPTA Regional Meeting in Costa Rica, developing a new Foundations in Transplantation pre-symposium for IPTA 2019, and contributing literature reviews to the newly established IPTA Quarterly Newsletter. The brand new IPTA Ethics Committee has established Ethics Cases which have been circulated in the newsletter in addition to carrying out an Ethics Survey – the results of which will be shared at IPTA 2019. The IPTA Outreach program has been completely revamped and received multiple applications for consideration. The IPTA Membership Committee reassessed and recommended a reduction in dues which took effect in 2018 in addition to establishing a Question Bank and undertaking other membership initiatives. The IPTA Nominations Committee facilitated the biggest election with the most number of candidates in IPTA history – the results of which will be announced at this meeting. The IPTA Awards Committee reviewed multiple award nominations for this year and these too will be presented during the Congress.
It has also been 2 years since I had the honour of starting my term as the president of the IPTA. The IPTA Council has worked hard on behalf of the association and are now embarking on a strategic planning process to establish the direction for IPTA for 2020-2023… stay tuned for more information.
I can truly say that it has been a pleasure and a privilege to serve this amazing organization. I remain awed by the commitment of IPTA members to children around the world in need of and following organ transplantation, and to each other as colleagues and friends.
I look forward to continuing to advocate for the children and IPTA as an organization and to continuing to grow together to achieve our common goals.
Sincerely,
Anne Dipchand
IPTA President

Would you like to include an event announcement in the newsletter? Some potential examples of this may include:
1. Event/meeting announcements
2. Job opportunities/postings
3. Requests for colleagues to join multi-center research collaborations
If you have any of these that you wish to include in the newsletter, please email to This email address is being protected from spambots. You need JavaScript enabled to view it.. Please note that in any announcement about events or job opportunities, no follow-up will be provided by IPTA – as such, full contact information for all of these events/opportunities should be included in the announcement. Please try to keep these relevant to the field of pediatric transplantation and pediatric organ failure.


Dear Colleagues,
On behalf of the IPTA Council we would like say Season’s Greetings. In warm appreciation of our Association during the past year, we extend our very best wishes for a happy holiday season!
Sincerely,
Anne I. Dipchand
IPTA President
Waiting for a liver
This case focuses on a 2-year-old girl with biliary atresia and failed Kasai. Over the past 6 months, she had become progressively worse, with mucosal and gastric bleeding episodically. She developed end stage liver disease and cirrhosis. Due to feeding intolerance with enteral feeds, a central venous line was placed and parenteral nutrition was started. She was listed for a liver transplant.
She was admitted to the hospital for electrolyte imbalances and fluid shifts. This hospitalization lasted for 5 months, due to GI bleeds, sepsis and general deterioration. She had issues with ascites, hypotension consistent with cirrhosis, spontaneous GI bleeds and 2 episodes of sepsis. (She had pruritus and constantly scratched at her central line dressing).
Mom stayed in the hospital with the patient and worried that her daughter would not make it to transplant.
She continued to demonstrate signs of decompensated cirrhosis: coagulopathy, ascites, and hypoalbuminemia/hyponatremia. She continued to have worsening labs, increased work of breathing and large amounts of bleeding from the central line site. She received multiple blood products to correct labs with no effect. She was oliguric secondary to hepatorenal syndrome and intravascular hypovolemia. She was increasingly agitated and distressed.
Her tenuous course worsened overnight. The parents spoke with the team and made the decision to change her resuscitation status to Do not resuscitate (DNR). Dad boarded a flight to the hospital, so that he could be at her side, when she passed away. A police escort to the hospital was arranged.
Thirty minutes after the DNR order was placed, the transplant surgeon received a call that a liver was available to the patient. The liver was a match for the patient. Since only 30 minutes had passed, the patient had remained listed for a liver.
Ethical questions: In the setting of “high risk” transplantation, it is very difficult to quantify risk factors. In this case, since the patient had been made DNR, she would die if the transplant did not occur. Would you tell the parents that an organ was available? Would you proceed to the OR?
Distributive justice: The patient did not survive the transplant. As we think about distributive justice, how to fairly divide resources, should the liver have gone to this patient? Without enough organs available for everyone who needs one, should the liver have gone to a patient who had a better chance of survival?

Application deadline: February 28th 2019
The IPTA is pleased to announce the renewal of its Outreach Program, established to support centers that seek to develop new solid organ transplant programs or to expand or enhance the quality of care in existing programs. The success of the Outreach Programs is enabled by enthusiastic participation of sponsoring programs, who will partner with applicant centers and can provide knowledge, expertise and education.
Transplant Program Standards Development: In order to better understand requirements for establishing and supporting successful transplant programs, the IPTA Outreach Committee has developed a set of simple standards that may be used to evaluate transplant program needs. These standards are meant to support the development of best practices in centers seeking support by the IPTA Outreach Program, but may also serve as a reference for programs seeking their own program development.
See the details regarding the Outreach Program guidelines and application process in the documents.
Click HERE for more details.
2018 Symposium in Organ Transplantation in Children in Review
The 2018 Bi-Annual International Pediatric Transplant Association Fellowship Symposium in Organ Transplantation in Children took place on November 12-13, 2018 at the Crowne Plaza Corobici San José, Costa Rica.
The special IPTA activity served as an educational forum for clinical and research fellows in pediatric solid organ transplantation, and other allied health professionals and trainees who are planning a career in pediatric transplantation. 80 participants joined from 20 different countries from Europe, Asia, Latin America, Africa and North America.
The intensive training course, led by council members of IPTA, awarded scholarships to international fellows to present their abstracts. 50 fellows submitted abstracts, and the education committee scored them blindly, 25 fellows were selected to participate.
For the first time ever, delegates were also invited to attend the symposium. They represented varying fields of pediatric transplantation including liver, lung, heart, psychology, psychiatry, adolescent medicine, and ethics among others. This diversity in content led to a very interactive experience and a high quality scientific program.
The scientific program was designed to deliver plenary lectures about broad aspects of transplantation, including immunology, vaccination, pre- transplant challenges and post- transplant complications of immunosuppression. There were interesting discussions that centered around case discussions on immunology issues, liver/intestine, heart/lung and kidney transplantation.
The presentations from the invited fellows were superb as they were well-prepared and led to engaging discussions. One such innovative and arousing session included a discussion on a potentially stunning way to increase donor supply “Organ donation after euthanasia in children and adolescents: Exploration of legal framework and medical suitability” by Jan Bollen and “Neonatal organ donation: A potential new donor source for cell and organ transplantation” by Emil Bluhme.
Faculty presentations were unique and insightful. Of particular note was the session of “Transplantation without Borders” whereby Mignon McCulloch’s talk “Pediatric transplantation in the developing world” and by J.P. Garbanzo who gave a candid and thoughtful lecture on the “Evolution of Pediatric Transplantation in Costa Rica”. Other lectures focused on advancing a career in pediatric transplantation with lectures that included writing grants and scientific articles for publication, as well as pursuing a well-balanced life in such a demanding field. The fellows were not afraid to engage with faculty and felt they built strong camaraderie with each other and the delegates. Trainees received feedback from the faculty, and enjoyed unique networking opportunities to discuss issues relevant to a career in pediatric solid organ transplantation.
The organization of the meeting was flawless both on the part of the IPTA organization team at The Transplantation Society, and the local IPTA organizers in Costa Rica. Dr. Olga Arguedas, CEO and Director of the Children’s Hospital in Costa Rica gave opening remarks and also planned a tour of the Hospital Nacional de Niños for all the participants. The symposium ended with the Fellows Dinner for everyone on at La Cascada Restaurant enjoying a typical Costa Rican dinner!


Want to stay up to date on transplantation? Want to test your knowledge? Here’s your chance!
The IPTA Question Bank is a new IPTA member benefit in which members will have access to new questions with each newsletter and access to additional questions and answers on the website. Each question will be accompanied by references to explain the correct and incorrect answers and it can be used as a teaching tool for students, residents and fellows as well.
Click HERE to procede.
Many of your members have been requesting information on how to access Pediatric Transplantation’s electronic table of contents. Below are instructions on how to subscribe now!
- Go to the Pediatric Transplantation homepage.
https://onlinelibrary.wiley.com/journal/13993046 - Ensure that you’re logged in with your IPTA access:
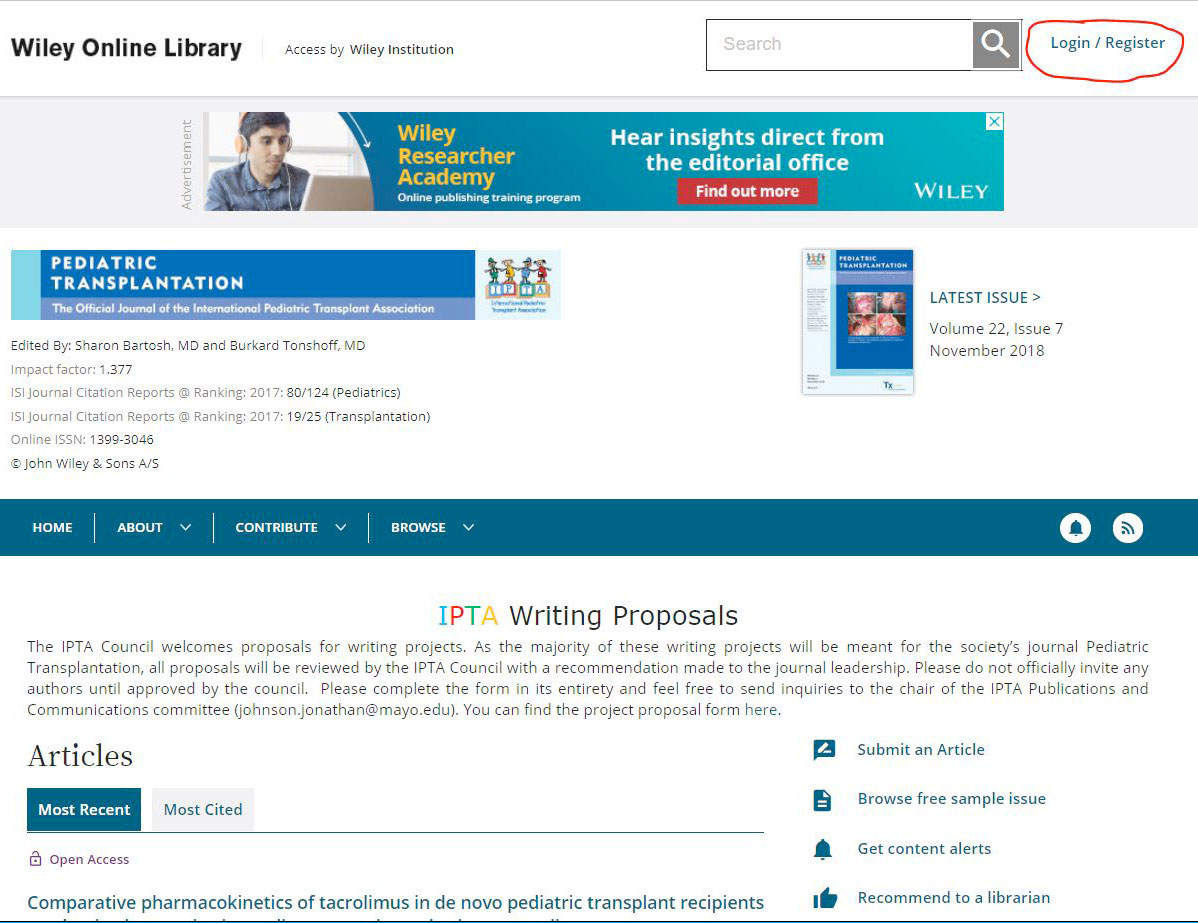
- On the right side of the page, click on Get Content Alerts:
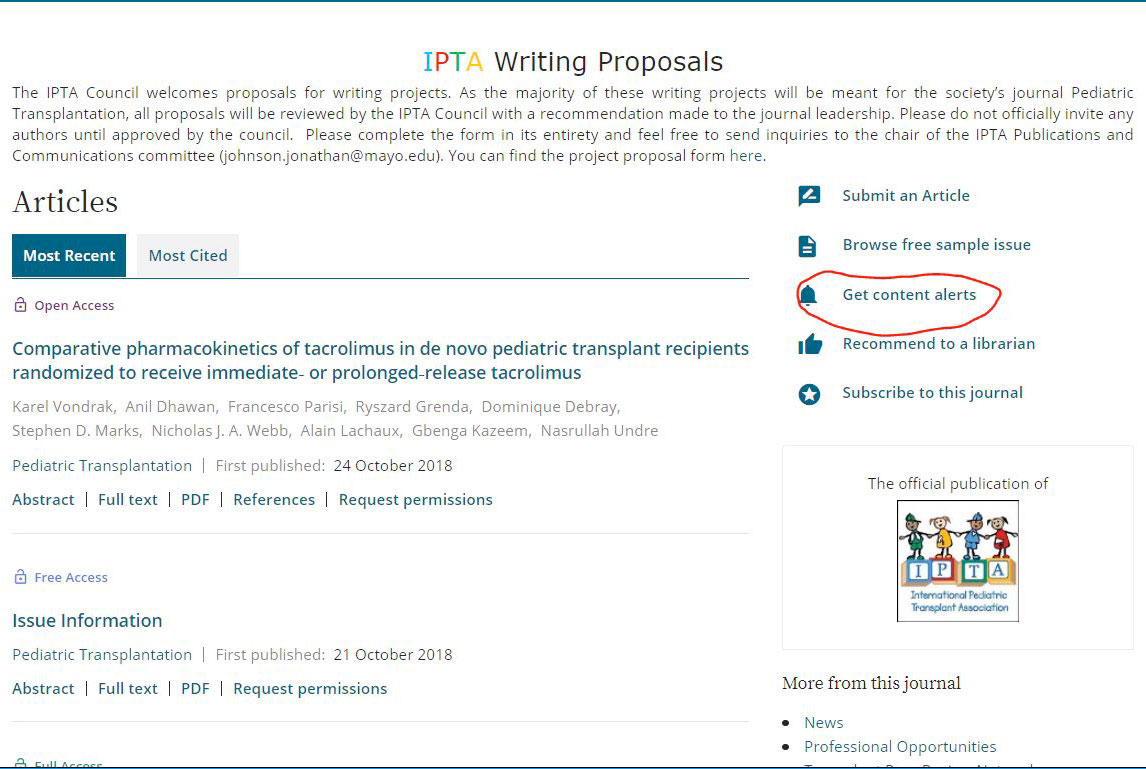
- You’re now subscribed! By default, you will receive an e-mail alert any time a new Pediatric Transplantation issue publishes as well as an alert any time new EarlyView (article published ahead of issue) content publishes. To change the frequency of EarlyView digest e-mails, click on the drop-down menu under Frequency and select
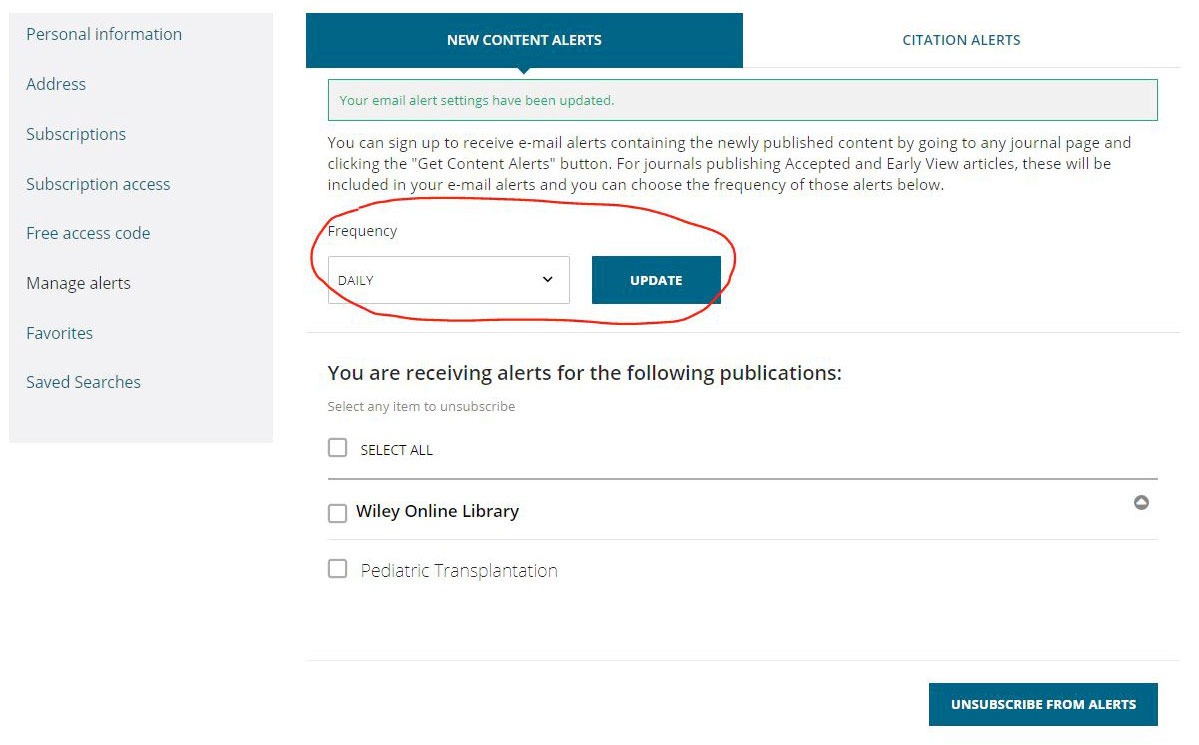
- To unsubscribe, check the box next to Pediatric Transplantation and select Unsubscribe From Alerts.

Registration fees are now posted on the website. You can go ahead and register for the main Congress, pre-meetings and social events.
Click HERE to register.

Newsletter Announcements – Open to the Membership
Would you like to include an event announcement in the newsletter? Some potential examples of this may include:
- Event/meeting announcements
- Job opportunities/postings
- Requests for colleagues to join multi-center research collaborations
If you have any of these that you wish to include in the newsletter, please email to This email address is being protected from spambots. You need JavaScript enabled to view it.. Please note that in any announcement about events or job opportunities, no follow-up will be provided by IPTA – as such, full contact information for all of these events/opportunities should be included in the announcement. Please try to keep these relevant to the field of pediatric transplantation and pediatric organ failure.


IPTA 2018 CALL FOR NOMINATIONS
The IPTA Nominations Committee is seeking qualified candidates to be considered for open Councilor and Officer positions beginning in May 2019.
All applications will be reviewed by the IPTA Nominations Committee, who will present a final slate of candidate Officers and Councilors to the IPTA membership for the 2019 election.
The IPTA Nominations Committee welcomes nominations and applications from anyone who has been an IPTA member in good standing for at least 1 year. Service to IPTA on committees or special activities relevant to the society is an asset.
The deadline for online submission of applications is September 30th, 2018.

10th Congress of the International Pediatric Transplant Association
The planning of the 10th Congress is well underway and we are thrilled with the list of speakers that have confirmed their participation! The Plenary and SOTA speakers are listed in the online preliminary program at ipta2019.org. International collaboration is an important part of the IPTA 2019 Congress. We have actively pursued opportunities to partner with other transplant and pediatric organizations across the world. It is important that we all work together as a community to advance the science and practice of pediatric transplantation. The Vancouver Congress will showcase collaborative sessions between IPTA and the following organizations: European Society for Organ Transplantation (ESOT); American Association for the Study of Liver Diseases (AASLD); American Society for Histocompatibility & Immunogenetics (ASHI); the International Society for Heart and lung Transplantation (ISHLT); American Society of Transplantation (AST); The Transplantation Society - International CMV Consensus Group; American Society of Pediatric Nephrology (ASPN); Canadian Blood Services (CBS); American Society of Transplant Surgeons (ASTS), and more to come.

This newsletter’s literary highlights come from David M. Briscoe, MD. MRCP. Director, Transplant Research Program, Boston Children's Hospital and the Department of Pediatrics, Harvard Medical School, Boston MA.
- Seifert ME et al. Subclinical inflammation phenotypes and long-term outcomes after pediatric kidney transplantation. Am J Transplant 2018; 1-11 [PMID: 29766640]
Despite improvements in short-term graft survival, long term outcomes following renal transplantation have not changed in over 20 years. One possibility is that standard clinical tests (e.g. creatinine and eGFR) only enable the diagnosis of intragraft disease once inflammation and fibrosis are present, which is more resistant to treatment. This is particularly relevant for pediatric kidney transplant recipients in whom creatinine-based eGFR is most imprecise because of the size mismatch between the child and the adult-sized kidney allograft. In this study, Seifert et al reported on the use of surveillance biopsies performed at 3 and/or 6 months post-transplant in a cohort of 120 pediatric recipients as a tool to identify subclinical inflammation (i.e. not detected using serum creatinine measurements). They also evaluated both the prevalence of pathological phenotypes seen on each biopsy and whether the use of surveillance had an impact on 5-year outcomes. This study represents one of the largest pediatric studies on surveillance biopsies to date. The major findings were: 1), that subclinical inflammation, either borderline or acute T cell-mediated rejection, was detectable in 36% of recipients by 6 months post transplant; 2), that the presence of subclinical inflammation in a surveillance biopsy is associated with increased risk for graft failure by year 5 post transplant; and 3), that treating subclinical rejection results in a better long-term outcome. They conclude that subclinical/borderline rejection is prevalent in pediatric recipients, that surveillance biopsies are safe and that intervention therapy has high potential to improve long-term outcomes. These findings also highlight the great need to monitor pediatric recipients with precision tools such as biomarker assays that support either the identity of high-risk patients or those recipients who are truly stable. It is also possible that precision biomarker assays may serve as a tool to identify pediatric recipients in need of surveillance biopsy. - Faddoul G et al. Analysis of Biomarkers Within the Initial 2 Years Posttransplant and 5-Year Kidney Transplant Outcomes: Results From Clinical Trials in Organ Transplantation-17. Transplantation 2018 Apr;102(4):673-680 [PMID: 29189482]
Several studies have demonstrated that increases in levels of the chemokines CXCL9 or CXCL10 in urine have a >70% sensitivity and specificity for association with intragraft inflammation/rejection. Their use as biomarkers has advantages to identify both low-risk stable patients as well as those at risk of graft failure. One of the larger studies evaluating urine biomarkers in the US enrolled 280 adult first kidney transplants as part of the NIH-sponsored Clinical Trials in Organ Transplantation (CTOT). This study revealed that urinary CXCL9 and/or other gene expression levels and assays including IFNy ELISPOT are excellent for detecting rejection. In the current study, Faddoul et al and the CTOT consortium reported the results of a follow up analysis of 5-year outcome data. Their analyses showed that early biomarker assays (within the first 2 years), including urinary CXCL9 levels, do not associate with long-term outcomes. In contrast, in this adult cohort they find that eGFR decline in the posttransplant period from 6 months to 2 years is a better surrogate of graft loss at 5 years. While this study highlights the utility of urine chemokine assays as biomarkers of rejection, it did not include pediatric recipients, in whom creatinine levels and eGFR are somewhat imprecise measures of early intragraft disease. - Mincham CM et al. Evolution of renal function and urinary biomarker indicators of inflammation on serial kidney biopsies in pediatric kidney transplant recipients with and without rejection. Pediatr Transplant 2018 Aug;22(5):e13202. doi: 10.1111/petr.13202. Epub 2018 Apr 25. [PMID: 29696778]
There is a great need to improve our ability to detect of subtle inflammation and subclinical rejection in pediatric renal transplant recipients. As discussed above (see Seifert et al), the use of surveillance biopsies can detect disease in over one-third of so-called ‘stable’ patients as assessed using standard creatinine-based clinical testing. This observation should serve as an added stimulus to advance the use of precision biomarkers in pediatric patients who are at risk of late diagnosis using current clinical assessment tools. To date, the search for reliable, sensitive and specific biomarkers has shown that the measurement of CXCL9 and CXCL10 in urine has high potential for utility as an early biomarker of intragraft disease. In this study, Mincham et al evaluated urinary CXCL10 levels in pediatric recipients as a follow up study from their group to evaluate longitudinal performance in the assessment of response to treatment. In this cohort, assays were performed at the same time as two consecutive renal biopsies, and urinary biomarker levels were correlated with pathology in a total of 49 biopsy pairs. Biopsy #1 was performed at a median of 11.7 months post-transplant and biopsy #2 was obtained 1.8 ± 0.8 months later. In their analysis the authors evaluated urinary CXCL10 levels as a ratio with urinary creatinine in order to enhance sensitivity. They also evaluated data on 134 unique metabolites according to a model previously reported by their group. Their major findings were: 1), that urine levels of CXCL10:Cr increase in association with rejection; 2), that levels decline ( P=0.01) following effective treatment of rejection; and 3), that low biomarker levels are present in patients without rejection. They also found that the metabolic measurements change directly in association with the degree of histological acuity on each biopsy. They conclude that urinary biomarkers associate with biopsy evidence of rejection in pediatric recipients, and that urinary levels of CXCL10:Cr are superior to serum creatinine as an index of histological disease.
Summary: Collectively, these three studies add strong support for the use of urinary biomarker assays as a precision tool in pediatric renal transplant recipients to identify: a), stable patients, b) patients in whom a surveillance biopsy is indicated, and c), to follow up the efficacy of an intervention treatment. Clinical trials are needed to further validate these possibilities and determine if the routine use of urinary biomarkers will advance care and outcomes in pediatric patients.

2019 IPTA Congress Awards
Nominations will open for the IPTA 2019 Awards on October 8. The selected candidates will be presented with their awards at the 2019 IPTA 10th Congress on Pediatric Transplantation.
IPTA Members are encouraged to nominate a colleague for any of the three awards being offered:
LIFETIME ACHIEVEMENT
Purpose: To recognize a member who has made outstanding contributions to the field of pediatric transplantation over the course of their career.
YOUNG SCHOLARS CAREER DEVELOOPMENT AWARD
Purpose:To recognize junior investigators who show scholarly promise, encourage them in their careers in pediatric transplantation and provide assistance to attend the IPTA Scientific Congress.
DISTINGUISHED ALLIED HEALTH MEMBER
Purpose:To recognize an Allied Health Professional member who has rendered years of faithful service to the Society and/or who has made a significant contribution to pediatric transplantation.

Outreach Committee Update
Outreach Program Renewal and Launch: The IPTA is pleased to announce the renewal of its Outreach Program, established to support centers that seek to develop new solid organ transplant programs or to expand or enhance the quality of care in existing programs. The success of the Outreach Programs is enabled by enthusiastic participation of sponsoring programs, who will partner with applicant centers and can provide knowledge, expertise and education. Details regarding the Outreach Program guidelines and application process can be found HERE
Transplant Program Standards Development: In order to better understand requirements for establishing and supporting successful transplant programs, the IPTA Outreach Committee has developed a set of simple standards that may be used to evaluate transplant program needs. These standards are meant to support the development of best practices in centers seeking support by the IPTA Outreach Program, but may also serve as a reference for programs seeking their own program development. They are meant to be adaptable to the specific circumstances of transplant centers around the world. These standards are being launched in association with the Outreach Program Renewal, and are available for reference on the IPTA website. We anticipate that these standards will need to be further refined and the Outreach Committee is looking forward to active feedback and is committed to updating the standards with input from the IPTA member community.
On behalf of the IPTA Outreach Committee
Tom D. Blydt-Hansen, MDCM, FRCPC
Associate Professor of Pediatrics, University of British Columbia
Director, Multi-Organ Transplant Program, BC Children’s Hospital

Dear IPTA Colleagues,
The overarching goal of the Peer Mentoring initiative is to facilitate and improve the quality of publications being sent by our membership to transplant journals, especially Pediatric Transplantation. One means of achieving this goal is to assist our membership, especially junior faculty and faculty from emerging transplant communities, in manuscript preparation. This will allow for these members to have dialogue with those experienced in the publication process prior to final submission.
We are seeking interested individuals who would be willing to help out with this new initiative. Responsibilities would include providing reviewer style feedback to the mentee prior to manuscript submission, and being available for subsequent questions. All members, including non-physician members, are encouraged to participate.
If interested, please send your name, email, and any specific areas of research focus to This email address is being protected from spambots. You need JavaScript enabled to view it..
Thank you in advance for your support,
Peer Mentoring Workgroup, IPTA
Chesney Castleberry, Workgroup Leader

Newsletter Announcements – Open to the Membership
Would you like to include an event announcement in the newsletter? Some potential examples of this may include:
- Event/meeting announcements
- Job opportunities/postings
- Requests for colleagues to join multi-center research collaborations
If you have any of these that you wish to include in the newsletter, please email to This email address is being protected from spambots. You need JavaScript enabled to view it.. Please note that in any announcement about events or job opportunities, no follow-up will be provided by IPTA – as such, full contact information for all of these events/opportunities should be included in the announcement. Please try to keep these relevant to the field of pediatric transplantation and pediatric organ failure.

Donate to IPTA Now! Your donation will be used to help IPTA to promote the advancement of the science and practice of transplantation in children worldwide and to serve as a unified voice for the special needs of pediatric transplant recipients.

The International Pediatric Transplant Association (IPTA) is a professional organization of individuals in the field of pediatric transplantation. The purpose of the Association is to advance the science and practice of pediatric transplantation worldwide in order to improve the health of all children who require such treatment. The Association is dedicated to promoting technical and scientific advances in pediatric transplantation and to advocating for the rights of all children who need transplantation.
Our Goals...
- Promote the advancement of the science and practice of transplantation in children worldwide
- Promote research and provide a forum that highlights the most recent advances in clinical and basic sciences related to pediatric transplantation
- Serve as a unified voice for the special needs of pediatric transplant recipients
- Develop educational programs for pediatric transplant professionals in underserved regions of the world that enable children to have access to transplantation globally
- Become the international leader in generating and disseminating information in the field of pediatric transplantation through the publication of our journal, Pediatric Transplantation
Who is IPTA?
President: Anne I. Dipchand, Toronto, CanadaPresident-Elect: Mignon McCulloch, Cape Town, South Africa
Secretary Treasurer: Carlos Esquivel, Stanford, USA
Past President: Burkhard Tönshoff, Heidelberg, Germany
Councilors:
Stephen Alexander, Sydney, Australia
David Briscoe, Boston, USA
Alan Langnas, Omaha, USA
Debra Lefkowitz, Philadelphia, USA
Stephen Marks, London, UK
George Mazariegos, Pittsburgh, USA
Lars Pape, Hannover, Germany
Klara Posfay-Barbe, Geneva, Switzerland
Katherine Twombley, Charleston, USA
Journal Editors:
Sharon Bartosh, Madison, USA
Burkhard Tönshoff, Heidelberg, Germany
Committee Chairs:
Michael Green, Pittsburgh, USA (Infectious Disease)
Jonathan Johnson, Rochester, USA (Publications and Communications)
Kenneth Brayman, Charlottesville, USA (Publications and Communications)
Louise Bannister, Toronto, Canada (Allied Health Professionals)
Beverly Kosmach-Park, Pittsburgh, USA (Allied Health Professionals)
Katherine Twombley, Charleston, USA (Membership)
Tom Blydt-Hansen, Vancouver, Canada (Outreach)
Rohit Kohli, Los Angeles, USA (Education)
Richard Trompeter, London, UK (Ethics)

You Can Make A Difference!
Dear IPTA Colleagues,
The Publications and Communications Committee is happy to announce a new Peer Mentoring initiative. The overarching goal of this new initiative is to facilitate and improve the quality of publications being sent by our membership to transplant journals, especially Pediatric Transplantation. One means of achieving this goal is to assist our membership, especially junior faculty and faculty from emerging transplant communities, in manuscript preparation. This will allow for these members to have dialogue with those experienced in the publication process prior to final submission.
We are seeking interested individuals who would be willing to help out with this new initiative. Responsibilities would include providing reviewer style feedback to the mentee prior to manuscript submission, and being available for subsequent questions. All members, including non-physician members, are encouraged to participate.
If interested, please send your name, email, and any specific areas of research focus to This email address is being protected from spambots. You need JavaScript enabled to view it..
Thank you in advance for your support,
Peer Mentoring Workgroup, IPTA
Chesney Castleberry, Workgroup Leader
The Ethics Case Series offers an open forum to share those cases we find ethically challenging in our own practice with the broader membership of our association. We would like to invite the membership of IPTA to assist us by submitting their own cases for inclusion in the IPTA newsletter’s Ethics Case Series to inform these discussions At this time there is no standardized format for submission, although we ask that you share your own insights into the cases you share. Please send your cases and thoughts about those cases to This email address is being protected from spambots. You need JavaScript enabled to view it. for consideration.
Michael Freeman, MD, MA (Bioethics)
Member, IPTA Ethics Committee
Ethics Case
A 12 year old male with a history of familial Hemophagocytic Lymphohistiocytosis (HLH), an immune deficiency disorder, was treated with an unmatched bone marrow transplant as an infant. Unfortunately, he developed graft vs. host disease (GVHD) after the bone marrow transplant, resulting in severe and progressive interstitial lung disease secondary to GVHD.
The parents pursued different treatment options for their son’s lung disease. He was ultimately listed for lung transplant. He had been relatively stable while listed, attending school 2 days/week. He was a very social boy and had many friends at school. He had an excellent understanding of his medical condition, a good sense of humor and overall social and cooperative demeanor. Parents were proactive and attentive and had the support of extended family that had assisted with both practical and emotional support over the years.
The patient also has mild gut and skin GVHD, GERD, seasonal allergies, nutritional insufficiency s/p G-Tube, chronic hypoxemia on 3-4L NC at baseline, and recurrent pneumothoraxes. He was admitted to the hospital in the setting of left sided pneumothorax s/p chest tube placement that was slow to resolve. The CT chest showed severe parenchymal and pleural fibrosis and several blebs, which put him at risk for further pneumothoraxes. The chest tube had an intermittent air leak, concerning for a possible bronchopleural fistula.
The patient's lung allocation score was > 50 when he was listed. Lung allocation scores range from 0-100, based on lab values, test results and disease diagnosis. There was no evidence of other organ dysfunction. Initially, he was ambulatory and hopeful. Since his score was quite high, it was hoped that he would receive lungs fairly quickly.
As the months passed, he remained on the waiting list and began experiencing significant, almost constant, coughing and dyspnea. A tracheostomy was placed as a bridge to transplant. He had difficulties in communicating easily after the tracheostomy and was frequently tearful, stating that he had been doing everything that the team had said and was not getting better. He had become increasingly frustrated with his prolonged hospitalization and need for more invasive procedures.
In the meantime, there was increased concern that his pleural disease has progressed to the point of making him a poor transplant candidate. His surgical risks were now much greater than in the past few months and the potential benefit had greatly decreased. It was felt that he would not survive transplant due to excessive bleeding. A team meeting was held and the decision was made to remove him from the lung transplant list.
When the team met with the parents about their son’s removal from the transplant list, the parents became very agitated and frustrated. The parents decided not to let their son know that he had been removed from the transplant list. They believed he would lose all hope if he learned that he is not listed. The parents were praying for a miracle. The team felt conflicted that the patient did not know that he had been taken off the list. However, the parent’s wishes were respected. He was discharged to a hospital closer to his home with a plan to limit interventions that would cause further discomfort. Symptom management was put into place to reduce his anxiety. He died 2 weeks later.
Ethics issues and challenges:
QUESTIONS TO CONSIDER:
Truthfulness and honesty: In the United States, patients under 18 years of age are considered minors. Before treating a patient less than 18 years of age, parents or legal guardians must sign consent to treatment. In decision making, parents are able to make decisions on behalf of their child, if they are less than 18 years old. In this case, should we honor the parents’ wishes, given that the patient had an excellent understanding of his medical condition? Does the decision of nondisclosure compromise values of transparency and respect for the patient (Bestor et al., 2018)?
Benefit of harm? The parents wanted to protect their son from the devastating news that he was no longer a candidate for lung transplant. The patient had been very involved and knowledgeable about his diagnosis and planned treatment. Was it in his best interest to be told that he was off the waiting list and would most likely die, so that he could prepare himself? Or, would telling the patient, against the parents’ wishes harm the family unit? If, as a healthcare provider, you are asked by the patient, “Am I dying?” would you collude with the parents?
Relational autonomy: This patient is not an adolescent; however the concepts of relational and in-control autonomy are to be considered. If this patient was 17 years old, would you go against the parents’ wishes and tell the patient that he was no longer a lung transplant candidate? Relational autonomy focuses on both the adolescent patient’s ability to make decisions, as well as the parents’ wishes. In-control autonomy does not focus on the adolescent patient’s participation, because the patient is not at an age where he is self-sufficient.
- Walter, J.W., & Ross, L.F. (2014). Relational autonomy: Moving beyond the limits of isolated individualism, Pediatrics, 133, S16-S23
- Bestor, J., Sabatello, M., van Karnebeek, C., & Lantos, J.D. (2018). Please test my child for a cancer gene, but don’t tell her, Pediatrics, 141, 1-7.
- Victor, A., George, C.E., Inbari, L.R. & Norman, G. (2018). Benefit or harm? A study on impact of collusion on the quality of life among palliative care patients, Indian Journal of Palliative Care, 24(1), 61-66.

Dear IPTA Colleagues,
We would like to invite you to attend the TTS 2018 Congress in Madrid, Spain from June 30 to July 5, 2018 and would like to especially draw your attention to the IPTA Pre-Congress Workshop on Sunday, July 1 from 14:00 to 17:30 which has some really exciting topics with which to update your knowledge in the following fields:
- Update of the Key Paeds Tx papers in the last 2 years in the fields of both Basic Science AS WELL as Clinical Transplantation – saves you having to read the papers!
- Discussion around the Tricky Concept of Adherence Intervention Trials
- What are the Tumour Risks following Pediatric Solid Organ Transplantation
- Metabolic Syndrome/Obesity – something we all face
Please make sure you have registered for the Pre-Congress Workshop as we would like to really have an interactive discussion. Also consider for those in Europe, sending your fellows – ideally for the whole congress – but even for the Post-graduate course on June 30 and July 1 – before the start of the Congress.
If you already registered to the TTS 2018 Congress and wish to add the IPTA Pre-Congress Workshop to your registration, please send an email to This email address is being protected from spambots. You need JavaScript enabled to view it..
If you have not registered yet and would like to attend the IPTA Pre-Congress Workshop onsite registration will be opened on June 30th.
We look forward to seeing you all there.
Best wishes,
Mignon McCulloch
Carlos Esquivel
On their behalf
TTS 2018 Congress Secretariat
27th International Congress of The Transplantation Society
505 Boulevard René-Lévesque Ouest, Suite 1401
Montreal, QC, H2Z 1Y7, Canada
IPTA 2018 Symposium in Organ Transplantation in Children
The International Pediatric Transplant Association is proud to feature a special Section activity: the 2018 Symposium in Organ Transplantation in Children: An educational forum for physicians, surgeons, and allied health professionals.
The focus of this symposium is aimed at clinical and research fellows in pediatric solid organ transplantation, as well as residents, and other allied health professional or non-physician trainees who are planning a career in pediatric transplantation.
The symposium will also provide state of the art information to established physicians, surgeons and allied health professionals who participate in the care of children before or after solid organ transplantation. In this case, a registration fee of $150/ person applies. Maximum capacity for established practitioners will be 50. THERE ARE 5 SEATS REMAINING TO REGISTER.

We continue to have an IPTA Member highlighting very recent publications in an area of general interest in the field of pediatric organ transplantation. This Newsletter’s Literacy Highlights come from Christian Benden, MD, FCCP, Medical Director Lung Transplantation, University Hospital Zurich and IPTA Education Committee Past Chair.
- Paraskeva MA et al. Outcome of adolescent recipients after lung transplantation: an analysis of the International Society for Heart and Lung Transplantation Registry. J Heart Lung Transplant 2018; 37: 323-331
Given the fact that recipient adolescent age is linked to inferior outcome after non-lung solid organ transplantation, Paraskeva from the Alfred Hospital in Melbourne, Australia, and an international group of co-workers utilized the largest thoracic transplant registry to date (International Society for Heart and Lung Transplantation Thoracic Transplant Registry) to investigate results of patients aged 10 to 24 years of age undergoing lung transplantation (LTX) between 2005 and 2013. Adolescent age has recently been defined as 10 to 24 years of age based on biologic and sociologic transitions happening in that age period. Almost 10% of the nearly 25,000 LTX patients in the Registry belong to the predefined adolescent age group. Overall, the survival in adolescents was significantly inferior compared to adults. In particular, the outcomes of adolescents aged 15 to 19 years of age were poorer compared to adults but also compared to all other pediatric age groups. Given these discouraging results in adolescent LTX recipients, it is paramount to improve particularly the transition of adolescents from pediatric to adult transplant services, strengthening self-care and decision-making of the adolescent. The data by Paraskeva and co-workers highlight again the urgency for further research in this area of transplant medicine that applies across all solid organ transplant types, with the aim to develop interventional tools to help to improve outcomes in this challenging patient group. - Urschel S et al. Neurocognitive outcomes after heart transplantation in early childhood. J Heart Lung Transplant (in press)
As outcomes following pediatric heart transplantation have markedly improved in the recent decade, non-somatic issues and health-related quality of life are increasingly important. Simon Urschel and colleagues from the University of Edmonton, Alberta, Canada, investigated neurocognitive capabilities in pre-school-age children either with congenital heart disease (CHD) or those failing anatomically normal hearts (CMP) undergoing heart transplantation (HTX) ≤ 4 years of age between 1999 and 2011. This prospective, multi-provincial project was based on data from the Complex Pediatric Therapies Follow-up Program in Canada assessing neurodevelopmental and quality-of-life outcomes in children in several Western Canadian provinces who require severe medical interventions in early childhood. The scores acquired from the multi-faceted cognitive assessment included the Wechsler Preschool and Primary Scales of Intelligence and a test of Visual-Motor Integration (VMI), scores obtained at 54 ± 3 months post-transplant. Of 76 study patients, 61 survived to assessment, and data of 55 children were finally included in the study results, N=32 with CHD and N=23 with CMP, respectively. Pre-transplantation, children with CHD were sicker spending more days on ventilators and undergoing more previous surgery, and the transplant operation required longer cardiopulmonary bypass time. Post-transplant, the mean IQ scores of all children were lower than the average and even significantly lower in children with CHD with more frequent intellectual disability; VMI was also reduced in the sub-group of children with CHD. Overall lower scores were correlated with a more complicated pre- and per-HTX path. Results of this study point out the importance of outcomes beyond sheer survival, focusing on non-somatic aspects and health-related quality of life. The need for close and continuous neurodevelopmental assessment is vital, and children and their families have to receive support based on individual requirements, psychosocial and financial, respectively. - Event/meeting announcements
- Job opportunities/postings
- Requests for colleagues to join multi-center research collaborations


Want to stay up to date on transplantation? Want to test your knowledge? Here’s your chance! Introducing a new IPTA member benefit, the IPTA question. Members will have access to new questions with each newsletter with additional questions and answers available on the website. Each question will be accompanied by references to explain the correct and incorrect answers. Can be used as a teaching tool for students, residents and fellows as well.
SUBMIT QUESTIONS TO ADD TO THE QUESTION BANK BY EMAILING This email address is being protected from spambots. You need JavaScript enabled to view it.
Click HERE to procede.
Electronic Table of Contents (ETOC). As a result of a recent platform migration, Wiley expects that IPTA members will be able to receive content alerts for Pediatric Transplantation without any action needed by the reader. In the meantime, if you’re not receiving new content alerts from Wiley about Pediatric Transplantation content, you’re welcome to by visiting the journal’s home page with your IPTA access and clicking “Get Content Alerts.”
Editorial board. Pediatric Transplantation is committed to establishing a rotation of members of the Editorial Board. The Editorial Board has recently been updated. As Editors-in-Chief, we express our gratitude to the previous Associate Editors for their service to the journal. Their contributions have helped shape the journal into something we are all very proud of. We are now working on the update of the other members of the Editorial Board. As IPTA is an international society, it is important to ensure global representation of the editorial board. If you are interested to serve on the editorial board, please send us your motivation and your CV with your academic accomplishments, This email address is being protected from spambots. You need JavaScript enabled to view it., This email address is being protected from spambots. You need JavaScript enabled to view it.
IPTA writing project proposal form. On behalf of the IPTA Council, we welcome proposals for writing projects. As the majority of these writing projects will be meant for the society’s journal Pediatric Transplantation, all proposals will be reviewed by the IPTA Council with a recommendation made to the journal leadership. This form is now available on the website of Pediatric Transplantation. Please send inquiries to the chair of the IPTA Publications and Communications committee, This email address is being protected from spambots. You need JavaScript enabled to view it..
CLICK HERE TO ACTIVATE CONTENT ALERTS FROM JOURNAL

Beginning with the next newsletter, we will be able to include announcements submitted by IPTA members for various events. Some potential examples of this may include:
If you have any of these that you wish to include in the newsletter, please email to This email address is being protected from spambots. You need JavaScript enabled to view it.. Please note that in any announcement about events or job opportunities, no follow-up will be provided by IPTA – as such, full contact information for all of these events/opportunities should be included in the announcement. Please try to keep these relevant to the field of pediatric transplantation and pediatric organ failure.

Donate to IPTA Now! Your donation will be used to help IPTA to promote the advancement of the science and practice of transplantation in children worldwide and to serve as a unified voice for the special needs of pediatric transplant recipients.
IPTA 2018 Symposium in Organ Transplantation in Children
The International Pediatric Transplant Association is proud to feature a special Section activity: the 2018 Symposium in Organ Transplantation in Children: An educational forum for physicians, surgeons, and allied health professionals.
The focus of this symposium is aimed at clinical and research fellows in pediatric solid organ transplantation, as well as residents, and other allied health professional or non-physician trainees who are planning a career in pediatric transplantation.
The symposium will also provide state of the art information to established physicians, surgeons and allied health professionals who participate in the care of children before or after solid organ transplantation. In this case, a registration fee of $150/ person applies. Maximum capacity for established practitioners will be 50.

Welcome to the introduction of the IPTA Ethics committee which is a new group that was formed at IPTA 2017 in Barcelona. We are currently working on a survey, which aims to explore the ethical issues within the paediatric transplant community across the world. This is based on original work in the adult transplant population through TTS and we have developed this for paediatric practice through IPTA.
We aim to survey those who are IPTA members or those who have attended IPTA conferences. We want to hear from all members of the multi-disciplinary teams and from all grades – even professors can give their opinion. However, any survey is only as good as the completed responses from the members and so we are very grateful to you all for spending time doing this survey.
Please find below the website address for the SurveyMonkey questionnaire.
COMPLETE THE SURVEYWe will let you know the results as soon as we have them available.
Many thanks for all your help,
Dr Stephen Marks, Consultant Paediatric Nephrologist and Principal Investigator
Dr Debra Lefkowitz, Co-Principal Investigator
Dr Richard Trompeter, Chair of IPTA Ethics Committee
Drs Anne Dipchand and Mignon McCulloch, IPTA President and President-Elect

With each newsletter, we will continue to have an IPTA member highlight important recent publications in an area of general interest. This newsletter’s literary highlights come from Rohit Kohli, MBBS, MS, Chief, Division of Gastroenterology, Hepatology and Nutrition, Children’s Hospital of Los Angeles.
- Allway R et al. (2017) Bioequivalence between innovator and generic tacrolimus in liver and kidney transplant recipients: A randomized, crossover clinical trial. PLoS Med; 14(11): e1002428.
Brand Tacrolimus vs. Generic Bioequivalence A recent study in PLoS Medicine reports on the bioequivalence between innovator (brand) and generic tacrolimus in adult liver and kidney transplant recipients. This was an 8 week randomized, crossover clinical trial with 35 renal transplant recipients and 36 liver transplant recipients. Within-subject variability was similar for the area under the curve (AUC) (range 12.11-15.81) and the concentration maximum (Cmax) (range 17.96-24.72) for all products. The within-subject variability was utilized to calculate the scaled average bioequivalence (SCABE) 90% confidence interval. The calculated SCABE 90% confidence interval was 84.65%-118.13% and 80.00%-125.00% for AUC and Cmax, respectively. Similar work in pediatric recipients is needed to address the specific pharmacokinetics of children and adolescents. - UHsu EK et al. Analysis of Liver Offers to Pediatric Candidates on the Transplant Wait List Gastroenterology. 2017 Oct;153(4):988-995. doi: 10.1053/j.gastro.2017.06.053.
Analysis: Pediatric liver offers on wait list in the USA A retrospective review of the US liver transplant wait-list over seven years resulted in identification of data for 3852 pediatric liver transplant recipients. To allocate liver donor organs to pediatric recipients the US system uses the Pediatric Endstage Liver Disease (PELD) scoring system and in addition a system for exceptions to the PELD is allowed through appeal. The authors report that amongst all the pediatric liver transplant candidates in the US that they reviewed, children who died or were delisted received a median 1 pediatric liver offer and waited a median of 33 days. Most importantly, of the children who died or were delisted, 45% died or were delisted with no offers. In a developed system such as that led by the United Network for Organ Sharing (UNOS) the death of a pediatric patient on the wait list with no offers is unconscionable. Therefore prioritization in the allocation for children and the future development of further improved risk stratification systems is required to eliminate wait-list mortality among children.


Want to stay up to date on transplantation? Want to test your knowledge? Here’s your chance! Introducing a new IPTA member benefit, the IPTA question. Members will have access to new questions with each newsletter with additional questions and answers available on the website. Each question will be accompanied by references to explain the correct and incorrect answers. It can be used as a teaching tool for students, residents and fellows as well.
Click HERE to procede.

Dear IPTA Colleagues,
The Publications and Communications Committee is happy to announce a new Peer Mentoring initiative. The overarching goal of this new initiative is to facilitate and improve the quality of publications being sent by our membership to transplant journals, especially Pediatric Transplantation. One means of achieving this goal is to assist our membership, especially junior faculty and faculty from emerging transplant communities, in manuscript preparation. This will allow for these members to have dialogue with those experienced in the publication process prior to final submission.
We are seeking interested individuals who would be willing to help out with this new initiative. Responsibilities would include providing reviewer style feedback to the mentee prior to manuscript submission, and being available for subsequent questions. All members, including non-physician members, are encouraged to participate.
If interested, please send your name, email, and any specific areas of research focus to This email address is being protected from spambots. You need JavaScript enabled to view it..
Thank you in advance for your support,
Peer Mentoring Workgroup, IPTA
Chesney Castleberry, Workgroup Leader

Career Development and Mentoring
While watching televised coverage of the Winter Olympics this year, my daughter asked me whether or not she could try the skeleton event. The skeleton, for those unaware, involves placing oneself on a sled and sliding down a bobsled track at speeds up to 80 miles/hr or 130 km/hr…. headfirst. My daughter is 5 years old. So, my typical parental answer of course was “maybe when you are older” – hoping she will forget and never ask me again. While thinking later about my answer, I realized that at some point, each one of those Olympic competitors had somebody say “yes” when they asked the same question and there was a team of people who identified their strengths and weaknesses, encouraged them, coached them, and they became Olympians.
All of us have difficult moments early in our careers: The first patient that presents in a way different from anything you saw during your training (if this hasn’t happened to you yet, trust me, it will happen). The first difficult decision that you had to make about whether or not to list a child for transplant, and the conversation that had to take place with the child and their family. The first time a patient had a poor outcome on your watch. Even making the decision to pursue highly specialized training in transplant medicine.
In all of these situations a mentor can be extremely valuable. Having someone to call to discuss that difficult patient, or serve as a sounding board when all isn’t going well in your position. The beautiful thing about pediatric transplantation, is that we are a small, tight-knit community of professionals who constantly work together to improve outcomes in children after transplant. During my first trip to an IPTA meeting, I had the opportunity to discuss difficult cases with senior colleagues in pediatric heart transplantation and have been fortunate to be able to foster these relationships: emails about difficult clinical situations, advice about a research project, career advice. There is no limit to the value of a good mentor.
I am proud to say that the different committees of IPTA all understand the value of good mentorship, and are all tackling this idea of mentorship for our members. The Education Committee is publishing quarterly literary highlights in this newsletter, bringing attention to important papers that may not have caught our attention in the prior 3 months. The Outreach Committee is working on assessing outcomes of IPTA outreach activities and finding the most effective ways to bring transplant expertise to as many children as possible. The Publications and Communications Committee is planning a Peer-Mentoring workshop at the next IPTA Congress in Vancouver, and is starting work on an official program for mentoring writers to facilitate and improve the quality of publications submitted to our journal. The IPTA Council and the Education Committee have continued to support education activities such as the 2018 Symposium in Organ Transplantation in Children, a meeting focused on educating junior faculty and trainees. Please see the top portion of this newsletter for more information about this amazing educational opportunity.
Starting your career in pediatric transplantation will be scary at times - there’s really no way around it. But, with a little help from your friends and mentors, we can continue to bring high quality care to the children of the world who need transplantation. Sometimes, all we need is someone to say “yes” and give us a little push down the track…
I look forward to seeing all of you in San Juan and in Vancouver!
Jonathan N. Johnson, MD
Co-Chair, Publications and Communications Committee, IPTA

Pneumosystis Jiroveci (PJP) Survey – Last Chance!
Pneumocystis jiroveci (PJP) remains an important pathogen among organ transplant recipients. While there are published guidelines for PJP prophylaxis following transplantation, in practice, there is likely wide variability in the individual approach to prophylaxis. To better clarify the current practice among transplant centers, we are conducting a survey to assess the use of PJP prophylaxis following pediatric solid organ transplant recipients. The link to the survey is included in this edition of the Newsletter. It is approximately 12 questions and should take fewer than 10 minutes to complete.
We appreciate you taking the time to COMPLETE THE SURVEY, and all responses will remain anonymous.Guidance on the Use of Live Vaccines in Solid Organ Transplantation

IPTA partnered in this recent highly successful collaborative initiative held in Toronto on Feb 22-23 with world-leading experts on live vaccine use in pediatric solid organ transplantation. The aim is to develop an international consensus protocol to include standards relating (but not limited) to immunologic evaluation pre-vaccination, timing pre- and post-transplant for vaccination, and the optimal safety surveillance system. We expect that the meeting will result in a document and publication that will be used widely around the world. Stay tuned for further updates!
Do not miss a single issue of Pediatric Transplantation! In order to get email reminders of new articles or issues, IPTA members must activate their journal content alerts. Click on the link below to log into your account and activate these alerts.



Donate to IPTA Now! Your donation will be used to help IPTA to promote the advancement of the science and practice of transplantation in children worldwide and to serve as a unified voice for the special needs of pediatric transplant recipients.
IPTA 2018 Symposium in Organ Transplantation in Children
The International Pediatric Transplant Association is proud to feature a special Section activity: the 2018 Symposium in Organ Transplantation in Children: An educational forum for physicians, surgeons, and allied health professionals.
The focus of this symposium is aimed at clinical and research fellows in pediatric solid organ transplantation, as well as residents, and other allied health professional or non-physician trainees who are planning a career in pediatric transplantation.
The symposium will also provide state of the art information to established physicians, surgeons and allied health professionals who participate in the care of children before or after solid organ transplantation. In this case, a registration fee of $150/ person applies. Maximum capacity for established practitioners will be 50.

Pneumosystis Jiroveci (PJP) Survey
Pneumocystis jiroveci (PJP) remains an important pathogen among organ transplant recipients. While there are published guidelines for PJP prophylaxis following transplantation, in practice, there is likely wide variability in the individual approach to prophylaxis. To better clarify the current practice among transplant centers, we are conducting a survey to assess the use of PJP prophylaxis following pediatric solid organ transplant recipients. The link to the survey is included in this edition of the Newsletter. It is approximately 12 questions and should take fewer than 10 minutes to complete.
We appreciate you taking the time to COMPLETE THE SURVEY, and all responses will remain anonymous.Ethical Case Request
Do you have cases that keep you up at night? Please share them with us!
Organ transplantation, particularly in children, is a process fraught with ethical questions. We routinely make decisions that can greatly impact our patients' lives with far from perfect information. How poor a prognosis does a patient have to have before he or she is no longer a transplant candidate? How should we weigh non-medical factors when making decisions? What allocation systems should we advocate for or emulate?
Just as encountering technically challenging cases can improve our clinical decision making, one way we can improve the ethical component of our care is by sharing those cases that keep us up at night, those cases we find ethically challenging in our own practice. We would like to invite the membership of IPTA to assist us by submitting their own cases for inclusion in the IPTA newsletter’s Ethical Case Series to inform these discussions. The Ethical Case Series, which debuted with September’s newsletter, offers an open forum to share these cases with the broader membership of our association.
At this time there is no standardized format for submission, although we ask that you share your own insights into the cases you share. Please send your cases and thoughts about those cases to This email address is being protected from spambots. You need JavaScript enabled to view it. for consideration.
Michael A Freeman, MD, MA (Bioethics)
Pediatric Nephrologist and Clinical Ethicist, Penn State College of Medicine, PA, USA
On Behalf of the International Pediatric Transplant Association Ethics Committee
Announcement of New Editors

IPTA is very grateful to Dr. Steven Webber for all of his service to IPTA. He was a founding Council member of IPTA, served as its third President, and for the last 5 years has served as Editor-in-Chief of Pediatric Transplantation.
Dr. Bartosh is a professor of pediatrics, Division Chief, pediatric nephrology and medical director of pediatric renal transplant at the University of Wisconsin, Madison, Wisconson. She has served on several IPTA committees and is currently active on the Education Committee. Dr. Tönshoff is a professor of pediatrics and pediatric nephrology, and the medical director of the pediatric renal transplant program in addition to being the Vice Chairman of the Department of Pediatrics at University Children’s Hospital, Heidelberg, Germany. He is currently past president of IPTA.
Drs. Burkhard Tönshoff and Sharon Bartosh will assume their roles as co-editors as of January 1, 2018. Stay tuned for more information in an upcoming editorial in Pediatric Transplantation.
Proposals for ipta-sponsored Writing Projects
The International Pediatric Transplant Association is dedicated to advancing the science and practice of pediatric transplantation worldwide, in order to improve the health of all children who require such treatment. To achieve this, part of our mission is to generate and disseminate information in the field of pediatric transplantation to our members and to the transplant community worldwide. This is primarily accomplished through the publication of important original research, review articles, commentaries and summaries to our journal, Pediatric Transplantation.
The journal leadership as well as the IPTA Council have and will continue to support our members in the creation of writing projects for the journal. We welcome proposals for IPTA-supported writing projects, including review articles, consensus documents, and other document types. All proposals will be reviewed by the Publications and Communications Committee, and reviews of the proposal will be provided to the author. Projects approved by the committee will then be reviewed by the IPTA Council with a recommendation made to the journal leadership. There may be overlapping ideas or project plans, and the committee will do our best to link up interested parties that may have similar proposals. Note that all projects will still have to undergo the standard peer-review process, and that not all projects will be approved.
On behalf of the members of the Publications and Communications committee, we look forward to working with you!
Please feel free to send us a note if any questions should arise - you can send inquiries to This email address is being protected from spambots. You need JavaScript enabled to view it.. We would be happy to informally discuss any potential ideas you may have at any time.
IPTA Infectious Diseases Committee Update
The IPTA Infectious Diseases (ID) Committee continues to be actively involved in generating information and guidance to benefit our members and the children that we care for. In many cases, members of the committee are collaborating with other members of IPTA to carry out these projects and develop manuscript and guidance. Amongst our current initiatives, the Committee is working with members of IPTA who participated in the 3rd TTS Consensus Conference on CMV this last spring to provide a pediatric perspective on the soon to be published updated CMV Guidelines. It is anticipated that this will follow a “Question and Answer” format and will be published in Pediatric Transplantation in 2018.
At the request of the IPTA Council, the ID committee has also recruited a group of experts to provide a review manuscript describing the role of emerging mosquito borne viruses (e.g. Zika, Dengue, Chikagunya) and their impact on organ transplantation. We again hope to see this manuscript published in Pediatric Transplantation in 2018. Finally, the ID Committee is working with Dr. Steve Webber to take on the leadership and organization of an IPTA-sponsored Consensus Conference on the Diagnosis, Management and Prevention of EBV Disease and PTLD in Pediatric Organ Transplant Recipients. It is anticipated that the working groups of the Consensus Conference will be meeting through much of 2018 with a goal of a face to face meeting to finalize recommendations sometime in the Fall of 2018.
Recent publications of interest in the arena of antibody mediated rejection
- Jordan, SC et al. IgG Endopeptidase in Highly Sensitized Patients Undergoing Transplantation. N Engl J Med. 377: 5: 2017
This is a report of 25 highly sensitized patients transplanted in 2 countries (Sweden, USA), with IdeS in an open label phase 1-2 trial of desensitization and transplant. IdeS, a cysteine protease, is an IgG-degrading enzyme derived from Step pyogenes. It is an endopeptidase that cleaves human IgG into F(ab’)2 and Fc fragments inhibiting complement-dependent cytotoxicity and antibody-dependent cellular cytotoxicity. Immunosuppression protocols differed significantly between the 2 countries. IdeS was shown to reduce or eliminate donor-specific antibodies and permitted HLA-incompatible transplantation in 24 of the 25 patients. There was a single allograft loss due to hyperacute rejection and 5 patients developed antibody mediated rejection. - Choi J., et al. Assessment of Tocilizumab (Anti-Interleuken-6 Receptor Monoclonal) as a Potential Treatment for Chronic Antibody-Mediated Rejection and Transplant glomerulopathy in HLA-Sensitized Renal Allograft Recipients. AJT. 17. 2017
This is a single center, open label report of 36 renal transplant patient with cAMR plus DSAs and transplant glomerulopathy who were treated as rescue therapy (progressive dysfunction having failed treatment with IVIg plus rituximab with or without PLEX), with monthly infusions of the anti-IL-6 receptor monoclonal antibody tocilizumab. Tocilizumab binds to both soluble and membrane-bound forms of the IL-6R and is approved by the FDA for treatment of rheumatoid arthritis and juvenile idiopathic arthritis. Significant reductions in DSAs and stabilization of renal function were seen at 2 years. Confirmation of this uncontrolled report, of course is necessary. - Clayton PA, Coates P. Are Sensitized Patients Better off with a Desensitization transplant or waiting on dialysis? Kidney International. 91. 2017
Although this article refers to 2 manuscripts (N Eng J Med: 374: 940-959. 2016 and Lancet; 389:727-734. 2017) which report conflicting results regarding the survival benefit of transplantation in sensitized adult kidney transplant patients, the questions addressed are not different for children. Wait for a well matched kidney or desensitize and attempt transplant??

| MEMBER LEVEL | 1 Year (USD) | 2 Years (USD) |
|---|---|---|
| Physicians | ||
| Trainees | ||
| Allied Health | ||
| Emerging Economy | $55 (USD) | $100 (USD) |
INVITE YOUR COLLEAGUES TO JOIN IPTA by forwarding this message!
4 GRAND PRIZES TO WIN!
For every referral, you get a chance to win one of three 2 year memberships or free registration to the IPTA 2019 congress!
In addition to reduced membership fees, there are lots of other important reasons to become a member of IPTA!
- Great opportunities to network and develop mentor/mentee relationships with other IPTA members. Networking opportunities include:
- The IPTA online member directory
- Symposium networking events
- Committee participation
- List-serve participation with questions specific to pediatric transplantation
- Up-to-date pediatric educational opportunities from the top leaders in the field of pediatric transplantation:
- Online subscription to the IPTA Journal: Pediatric Transplantation
- Discounted journal subscription rates for Transplantation, Transplantation Proceedings and Transplantation Reviews
- Biennial Fellows Workshops (The 2018 workshop will be held in Costa Rica)
- Access to the IPTA 2015 and 2017 Congress recordings
- Reduced Congress registration fees for the 2019 Congress in Vancouver
- Trainees and Allied Health members are eligible to apply for travel awards for the biennial Congress
- The IPTA quarterly newsletter that includes:
- Case studies dealing with key ethical issues to spark awareness, education and discussion
- Literature reviews
- Committee initiatives and updates
- And so much more!
- A $50 discount off The Transplantation Society (TTS) dues when paying IPTA and TTS dues at the same time
- Become involved in one or more of IPTA’s very active committees for even more networking and educational opportunities. There are several to choose from including: Allied Health, Membership, Ethics, Education, Infectious Disease, Outreach, and Publications and Communications
Become a leader in the field of pediatric transplantation by your active involvement in the International Pediatric Transplant Association!

IPTA 2017 Congress

The 9th Congress of the International Pediatric Transplant Association (IPTA) took place in Barcelona, Spain, from May 27-30, 2017 and was a great success both in terms of its excellent attendance and its scientific quality. Topics being addressed were updates and new data from ongoing pediatric transplant clinical trials (CTOTC), long-term complications following transplantation, standards for surveillance and treatment of infections in transplantation, perspectives in immune tolerance, up-to-date data from important registries, new and emerging immunosuppressive agents, ethical dilemmas in pediatric transplantation, devices used to support transplantation, issues in noncompliance and transfer of care, just to name a few.
There were special sessions designed for allied health-care professionals (AHP), who have a strong international AHP community within IPTA. The IPTA Lifetime Achievement Award was bestowed post-humously to Dr. William Harmon, and the Pioneer in Transplantation Award to Dr. Benedict Cosimi. Attendees from around the globe had the opportunity to network and plan for future clinical and research collaboration.
Ethical Case Studies
IPTA is pleased to introduce Case Studies dealing with key ethical issues in our quarterly newsletters to spark awareness, education and discussion. These will be spearheaded by the IPTA Ethics committee.
Case Study 1
Introduction
An eight-year-old girl with end-stage kidney disease secondary to Finnish type congenital nephrotic syndrome initially managed with daily albumin infusions requiring peritoneal dialysis from nine months of age followed by bilateral retroperitoneal nephrectomies at ten months of age. In her first two years of life, she had numerous treatment-related problems including multiple episodes of sepsis, requiring changes of central venous catheters; a chronically leaking gastrostomy (which eventually was removed) and severe gastro-oesophageal reflux disease, hypothyroidism, renal osteodystrophy and hypertension secondary to fluid overload. Following several episodes of severe peritonitis, including MRSA peritonitis, her peritoneal dialysis catheter was removed and subsequently an abdominal collection was drained. Haemodialysis was then commenced, but venous access proved to be difficult and became increasingly so over the forthcoming months.
A venogram revealed many occluded and stenosed veins; the thromboses in the superior vena cava and subclavian veins were identified as compromising catheter patency. At 19 months, she was admitted urgently to hospital with physical signs of acute sepsis (fever, tachycardia) associated with marked abdominal distension and tenderness. She failed to respond to standard antibiotic therapy and was found to have vegetation on the tricuspid valve within the right ventricle, suggestive of infective endocarditis, but without evidence of pulmonary emboli. She was treated with six weeks of intravenous antibiotics, and a permanent haemodialysis catheter was inserted. At this stage, our patient had suffered episodes of severe MRSA peritonitis associated with staphylococcal bacterial endocarditis, necessitating the removal of her peritoneal catheter; peritoneal dialysis was no longer an option. Haemodialysis was also problematic because of extreme difficulty in vascular access; it also became apparent that a vascular graft for haemodialysis would not be successful.
Unfortunately, there were no transplant options as she had been on call for over a year for a deceased donor and there was no living donor as her mother could not donate for medical reasons and her father, although a suitable match, stated he was unable to donate.
- What medical care options exist for this patient?
- What are the ethical considerations?
The lack of effective dialysis or transplant options made both practical management and prognostication difficult and raised significant ethical dilemmas for the professionals concerned with her care. Following extensive meetings involving the intensive care team, the multidisciplinary team, close family members and the clinical ethics service, agreement was reached that an ethically appropriate action was that she should receive symptom care management at home and that no further active life-sustaining treatment should be offered.
Although she was discharged on these terms, the ethical debate did not cease. It transpired that the father had told his wife and family that the healthcare team had said he was an unsuitable donor. Although this was certainly not the case, the healthcare team felt unable to tell the family, because to do so would have been to breach the duty of confidentiality owed to father. Matters became further complicated when the parents requested resumption of full active management and other members of the wider family became involved. The latter requested copies of the patient’s notes, including all the pre-transplant work up and asked the specific question, “Why won’t you let her father donate?”
Contrary to expectations the child’s overall condition improved at home while receiving no fluids or therapies, so that she became more like the happy and playful child she had previously been. Her father reported that this change was more than he could bear and that in consequence he now wished to donate his kidney and moreover he did so freely. This was an unusual turn of events, but the team felt on reflection on the ethical issues, that they had little option but to respect the father’s wishes. The patient was accordingly recommenced on haemodialysis and the father underwent a full work up, including a psychiatric assessment, prior to kidney donation three weeks later.
Ethics Commentary
In deciding what treatment might be offered to this child it was crucial to ascertain what her best interests were and how, and by whom, they should be determined. The child had already had extensive medical treatments, requiring considerable time in hospital, and realistic therapeutic options were very limited. From a clinical perspective, there was clear consensus that renal transplantation was in the child’s best interests, in that it provided her with the best opportunity for an open future and would be likely to enhance quantity and quality of her life. Analysing the girl’s wishes and preferences was not possible to the extent required for her to determine her own future but the parents were clear that they wanted their child to survive and wanted her to receive the necessary treatment to prolong her life. Considering contextual factors (such as family’s social circumstances beliefs and values, they did not alter the apparently agreed view that renal transplantation was in her best interests.
However, the likelihood of a deceased donor organ becoming imminently available was considered unlikely and this led to an urgent scheme being introduced for potential paediatric renal transplant recipient. The clinical team worried about the burden of continuing dialysis in a girl in whom the medium or long-term options for this were effectively closed by poor access. Although the father was a match for live organ donation, he had stated that he did not wish to donate a kidney despite understanding, in the abstract at least, the consequences for his daughter if he did not. The treating team were ethically troubled by this as they felt that their primary duty was to the child, their patient. Nevertheless, they also recognised that they had an ethical and legal duty to respect the father’s apparently autonomous choice, even though they felt that his decision was not in the best interests of his child. A decision to force him to donate, even though it would have prevented harm to his daughter, could have been regarded as a disproportionate response with respect to his right to exercise a free choice. Given this analysis, and the certainty of death from end-stage kidney disease without transplantation or effective dialysis it seemed that the child’s best interests could only be served by the provision of high quality symptom care management to support her and her family and to ensure that her death was as peaceful as possible. In that sense, the decision to discharge was an ethically justifiable one.
However, ethical dilemmas for the treating team did not stop at that point. The child’s condition improved when she got home so that a request to resume active treatment was made. The team felt that such a request was only ethically sustainable if it were to lead to transplantation with her father as the live donor. The team were also aware that her father had told the immediate family that it was the clinical team who had decided he was an unsuitable donor. When confronted by the extended family’s request for information and a specific question as to why they had rejected the father as a donor, the team had the option of telling the truth to the family, or fulfilling their duty of confidentiality to the father. An analysis of the likely consequences of either course of action led them to the conclusion that the best interests of the child were more likely to be served by non-disclosure.
In the event, after long discussions with the father himself who saw that his child was dying, he changed his mind and offered himself as a donor. However, given the family circumstances and the involvement of the extended family the team could not be sure that his choice was freely made and that he had not been subject to such coercion as to make his consent to donate invalid. It could also have been the case that the father had come to believe that donation was the action that would define a virtuous father and one that would lead to an overall flourishing of the family unit, and thus be in accordance with principles of virtue ethics. Moreover, the outcome of her father’s donation was one that professionals and family alike considered to be in the child’s best interests and one that in practice was to eventually produce the desired outcome for her. In these circumstances, it seemed ethically appropriate, if not legally required, to have a psychiatric assessment. Overall the case illustrates the importance of process as well as outcome in the resolution of ethically challenging dilemmas and the complex interweaving roles of moral principles in the process.
Case Study 2
A 3 year old girl was diagnosed with nephrotic syndrome secondary to FSGS. She was initially treated with steroids and Cytoxan later converted to cyclosporine A. Despite treatment she slowly deteriorated into ESRD and started dialysis. At 10 years of age, she underwent a deceased donor kidney transplantation and was managed with triple immunosuppressive protocol (CyA, MMF and steroids) without pre-transplant plasmapheresis (PP).
At the 14th post op day with creatinine levels dropping to 1.0mg/dL she developed proteinuria of 17g//24hr. and was placed on PP sessions 3 times/ week followed by Rituximab (single dose of 375mg/m2). The following months despite aggressive continuous sessions of PP maintaining her protein urine level <10g/day she developed hypoalbuminemia (albumin levels 2.2g/dl) associated with severe leg edema, skin infection and convulsive disorder secondary to PRESS. At six months after transplant her mother requested to discontinue immunosuppressive treatment and she returned to dialysis.
Six years later she was fed up with dialysis and asked to be listed for a second transplant.
- At this stage would you consider a second transplant using one of the parents who was a match donor knowing that this scenario might be associated with a high risk of recurrence?
We thought that we shouldn't offer live donation and listed her for a deceased donor transplantation. She had a PRA of 60% and waited almost 9 years until she received her second transplant. Rituximab was given as part of the induction protocol and PP was initiated at the second post-op day as a preventive measure. Despite these measures on post-op day 7 she developed again a high level proteinuria of 14g/24hr. She continued with PP sessions X3 for another two weeks followed by gradual reduction of the PP interval to once a week. Again, she presented with a full spectrum of complications secondary to severe proteinuria including anasarca, abdominal fluid collections requiring drainage to relieve abdominal tension and hypoalbuminemia.
- Is there any benefit to continue PP and maintain the graft?
- Should we give her a chance of a third transplant with our current inefficient treatment for recurrent FSGS?
Literary Highlights
With each newsletter, we plan to have an IPTA member highlight important recent publications in an area of general interest. Since all our members have access to our journal PEDIATRIC TRANSPLANTATION, this feature will highlight reports, from other journals, which may not be readily available to all our members. As with this inaugural edition, reports of adult data that may have relevance to our members may also be included. This newsletters’ literary highlights come from Sharon Bartosh, M.D., Chief, Pediatric Nephrology, American Family Children’s Hospital, University of Wisconsin.
- Allen PJ et al. . Recurrent glomerulonephritis after kidney transplantation: risk factors and allograft outcomes. Kidney International; 92: 461-469, 2017.
- Cosio FG and Cattran DC. Recent advances in our understanding of recurrent primary glomerulonephritis after kidney transplantation. Kidney International; 91: 304-314, 2017.
- Pippias M et al. Long-term kidney transplant outcomes in primary glomerulonephritis: Analysis from the ERA-EDTA Registry. Transplantation; 100: 1955-1962, 2016.
IPTA Committees 2017-2019
Much of the work of IPTA is can only be done through the contributions of our committees. We would like to introduce you to the IPTA committees for 2017-2019 and share their current initiatives.
Allied Health Professional (AHP) Committee
2017-2019 Initiatives
The AHP committee is in the process of carrying out a survey to describe the demographics and interests of transplant allied health professionals. The goal is to determine how the allied health committee can encourage and increase IPTA membership, as well as foster a greater involvement in allied health activities and committee work within the organization. The committee will revise and expand the Allied Health Professional page on the IPTA website to include a mission statement, a description of the AH community in transplant and their specific roles in caring for pediatric transplant patients, committee initiatives, membership benefits, quotes from members and how to become a member. The committee also plans to explore a link for networking and the ability to post questions to other AH members. The committee plans to develop an article for publication in Pediatric Transplantation on a contemporary topic that is relevant to the AHP community in addition to participating in review of the UNOS parent manual.
Education Committee
2017-2019 Initiatives
The Education committee has already participated in the IPTA review of the UNOS parent material and is in the process of a survey related to the Postgraduate Course of the IPTA 9th Congress in order to inform further course development. The Education committee will be developing the curriculum for the IPTA Fellows meeting in November 2018 and the renamed postgraduate course “Foundations in Transplantation” for the IPTA 10th Congress in Vancouver in 2019. Other exciting initiatives will be forthcoming this Fall.
Ethics Committee
2017-2019 Initiatives
The Ethics committee is the newest IPTA committee that has been formed to address the increasing ethical awareness in pediatric solid organ transplantation. As they develop their initiatives as a new committee, the group plans to raise awareness and educate by contributing cases to the IPTA newsletter (see this issue of the newsletter for their first contribution). In addition, to build upon a recent TTS initiative, they will be editing the recent TTS Ethics Survey for pediatrics with a goal to circulate it in early 2018 and to use the information gathered as a foundation for further initiatives moving forward.
Infectious Disease Committee
2017-2019 Initiatives
The ID committee has a number of active initiatives involving assessing current practice and developing consensus recommendations for publication in Pediatric Transplantation including 1) evaluation and approach to the presence of active infection in the potential pediatric transplant recipient, 2) status of the use of live vaccines after pediatric solid organ transplantation, and 3) pneumocystis prophylaxis strategies, in addition to a yearly Influenza Update. The ID Committee is proposing to develop a commentary to the TTS CMV Guidelines (currently in progress) specific to the pediatric perspective. This would highlight changes to both the overall document as well as to the pediatric section and its recommendations. In addition, the Committee hopes that the proposed commentary could identify ongoing pediatric specific gaps in the data with a goal of hoping to target future. Looking ahead, the ID committee is exploring the development of PTLD practice recommendations potentially including diagnosis, management and prevention. These are just some of the exciting initiatives coming out of the ID committee.
Membership Committee
2017-2019 Initiatives
The Membership Committee will be exploring a new dues structure for IPTA which is long overdue. This will take into consideration many different factors including our diverse membership of an international nature, the need to foster collaboration at all levels of pediatric transplantation, the need to develop junior people to pursue pediatric transplantation, and administrative considerations including the transition to TTS as a section and the move to an online journal. The Membership committee with also be looking at how to enhance the value of IPTA membership, focusing on member renewal and retention, and recruitment of new members – especially junior members and allied health professionals.
Outreach Committee
2017-2019 Initiatives
The Outreach committee is in the process of revising its mission, purpose and the application guidelines, processes and procedures - all of which will be made available to the IPTA membership when completed and approved by the IPTA Council. The committee has recently reviewed the status of the past projects and will provide a summary for the IPTA newsletter this year in addition to putting information on the IPTA website. The recent projects in Sri Lanka and Cape Town are in the process of being reviewed. In 2018, the committee will spearhead a call for a new round of applications following consolidation of all of the abovementioned initiatives. Stay tuned for more information!
Publications and Communications Committee
2017-2019 Initiatives
The Publications committee is going to assume a central role in increasing the publications from IPTA members in Pediatric Transplantation using a number of different strategies. Some of these include iincreasing the number of publications coming from committee members, increasing the number of authors involved in IPTA-sponsored writing projects, expanding the scope of writing projects to include white papers and practice recommendations, and working with other IPTA committees on joint projects. The Publications committee plans to work on a Peer Mentoring program to help authors with backgrounds in languages other than English, to improve the quality of the language of their submissions. Finally, the Publications committee will take a leadership role in the quarterly IPTA newsletter, working with the other committees to provide content that is interesting and relevant to the IPTA membership.

Seasons Greeting from IPTA President
Dear IPTA members, colleagues and friends,
The IPTA Executive, Council and Committees are pleased to provide you with the third Newsletter this year for an update of our Association's activities. We will give you an overview on the projects and initiatives of the Allied Health Committee, Publication Committee, Membership Committee and Awards Committee with information on the newly introduced IPTA-TTS Congress Scientific Awards for trainees, allied health professionals and members from emerging countries. Most importantly, the IPTA 2017 Congress Chair Anne Dipchand will give an update on the upcoming 9th Congress of our Association in Barcelona, Spain, from May 27-30, 2017. The Scientific Committee has developed an exciting program that meets the needs of participants from across the world.
I look forward to seeing many of you at the upcoming IPTA Congress. Until then, feel free to reach out to me at any time with IPTA-related questions or comments. I always appreciate hearing from you.
Lastly, I would like to thank everyone for your engagement and support of the IPTA, wish everyone a relaxing and peaceful holiday season!
Yours sincerely,
Burkhard Tönshoff
IPTA President
Membership Committee Update
The Membership Committee has been active in working to recruit new members to the Association. In particular, to take advantage of the Barcelona meeting to broaden the membership in Europe and Asia. Steps have been taken to clarify the membership form and improve the capacity to pay for membership on-line.
The benefits of membership regarding the journal and awards and meetings has given us increased opportunities for recruitment.
We are hoping in the next six months leading up to the Barcelona meeting to address initiatives to increase the membership of junior trainees, researchers and young faculty and broaden membership amongst allied health and nursing.
We are happy to receive any ideas for the Membership Committee and any interested members who would like to join the Committee.
Stephen Alexander
Membership Committee Chair
IPTA Publications Committee Update
The IPTA Publications and Communications Committee is responsible for developing various publications relevant to IPTA members for publication in Pediatric Transplantation, the official journal of the IPTA. The Committee met recently to discuss future publications but would welcome feedback from members on topics they feel would be important for consideration, comments can be sent to This email address is being protected from spambots. You need JavaScript enabled to view it..
We are also pleased to welcome our new Committee members: Richard Kirk, cardiologist from Texas, Erika Pace, liver transplant specialist, Mariastella Serrano, liver transplant specialist, Manuel Rodriguez-Davalos, Director of the pediatric transplant unit in New Haven, Kenneth Brayman, transplant surgeon, Charlottesville, and Ryan Fischer, liver transplant specialist, Kansas City.
Guido Filler
Publications Committee Chair
Allied Health Committee Update
The Allied Health Committee is excited to announce our new members. First, joining us a Co-Chairs elect are Louise Bannister from Toronto, ON, CA and Beverly Kosmach-Park from Pittsburgh, PA, USA. They will take over as co-chairs at the Congress in May, and we are excited for their enthusiasm to lead this Committee moving forward. Other new Committee members include Christine Divens (Clinical Nurse Specialist, Pittsburgh, PA, USA), Barbara Roessner (Physician Assistant, Omaha, NE, USA), Luca Dello Strologo, (Nephrologist, Rome, Italy), Laura O’Melia (Nurse Practitioner, Boston, MA, USA) and Karyn Sanson (Nurse Specialist, Auckland, NZ). This group joins our continuing members Debra Lefkowitz (Psychologist, Philadelphia, PA, USA; outgoing Chair and current IPTA Councilor), Dawn Freiberger (Nurse Coordinator, Boston, MA, USA), Jo Wray (Psychologist, London, UK), Diana Shellmer (Psychologist, Pittsburgh, PA, USA).
The AHP Committee is currently examining some new initiatives. Our first project is to survey our membership to gain a better understanding of group interests, project ideas, and preferred communication methods. We’ve seen tremendous enthusiasm from our Allied Health colleagues at prior Congresses, and want to figure out how to better harness this energy and foster international connections between this very diverse group of people. Other proposed projects include additional monographs for Pediatric Transplantation as well as position papers and best practice guidelines.
Debra Lefkowitz
AHP Interim Committee Chair
IPTA PRESIDENT’S MESSAGE
Dear IPTA members, colleagues and friends,
The Executive Committee, the Council and the IPTA committees are pleased to provide you with the second Newsletter this year for an update of our Association's activities. We will give you a comprehensive update on the projects and initiatives of the Education Committee, Infectious Disease Committee, Publication Committee, and the newly founded Ethics Committee. We are delighted that 24 IPTA members recently volunteered for collaboration in these committees! It is a good way to involve the membership and to increase the interaction with the transplant community.
The upcoming 26th International Congress of the Transplantation Society (TTS) will be held in Hong Kong from August 18-23, 2016. There will be various IPTA activities during the congress such as an IPTA/TTS Pediatric Post Graduate Course on August 19, 2016 focusing on two major topics: “Listing children for solid organ transplantation and donor selection” and “Specific aspects of post-transplant care in children” and two scientific sessions organized by IPTA. Hopefully you will have the chance to join this important congress with our mother society TTS. Please stop by for a chat; all of your suggestions are welcome. Have a great summer!
Yours sincerely,
Burkhard Tönshoff
IPTA President
IPTA 2017: A CONGRESS OF COLLABORATIONS!
Anne I. Dipchand, Congress ChairEIGHT MONTHS TO GO … and it will go by so quickly! Program planning is well underway and we are thrilled with the response and enthusiasm of our invited speakers! Look for a preliminary program to be online later in 2016.
Collaboration is an important part of the IPTA 2017 Congress. On the springboard of our partnership with TTS, we have actively pursued opportunities to partner with other transplant organizations. It is important that we all work together as a community to advance the science and practice of transplant medicine, especially the pediatric component through IPTA. The Barcelona Congress will showcase collaborative sessions between IPTA and the following organizations:

We are very excited about the opportunity to work together with these international transplant societies and believe that this will be the beginning of future partnerships allowing us to advance pediatric offerings moving forward. We continue to work with other organizations and hope to add to this list over the next few months.
Every society is as strong as its members, and the same can be said for IPTA. You will soon receive requests for nominations for the IPTA biennial awards. We look forward to your nominations of your colleagues around the world so that we can honor them for their dedication to pediatric transplantation. This year we will also announce the first IPTA Pioneer in Transplantation lecture and award to a well deserving pioneer in our field.
As you plan your trip to IPTA 2017, here is a recap of other things to look forward to: a vibrant Opening Ceremony on Saturday May 26th; scientific sessions that will include world renowned plenary and state-of-the art speakers; and the very popular parallel interactive workshop sessions with experts in the field. Experience the history of medicine in Spain at the Hospital San Pau during the congress social evening on Monday May 28th.
PEDIATRIC ORGAN TRANSPLANTATION SUMMER SCHOOL
ZAVIDOVO, RUSSIA
The IPTA Executive Committee and two former presidents of IPTA, Drs. Richard Fine and Richard Trompeter, had the opportunity to participate in the recent Pediatric Organ Transplantation Summer School, organized by Drs. Michael Kaabak and Nadeen Babenko of the Petrovsky Research Center of Surgery in Moscow. Two days of in depth discussions covering all aspects of pediatric kidney, heart and liver transplantation were presented to an audience of some 150 pediatric transplant specialists, mostly nephrologists and surgeons from all over Russia. The venue was near Tver, an hour north of Moscow. The talks were well received, with questions and discussion from the audience and among the speakers.
he pediatric kidney transplant program in Russia is the largest pediatric kidney transplant program in Russia, and performs some 30 transplants in children annually; it is the only program in Russia transplanting kidneys into small children under 5 years of age.

Ron Shapiro, Anne Dipchand, Mignon McCulloch and Burkhard Tönshoff
EDUCATION COMMITTEE UPDATE
Chair: Christian Benden, Switzerland
Incoming Chair: Rohit Kohli, OH, USA
The Education Committee, an international group of pediatric transplant physicians/surgeons and allied health professionals, is responsible for expanding IPTA's educational activities. In 2016, the Education Committee has continued to expand the Society’s educational activities co-organizing the biennial IPTA Fellows Symposium on Pediatric Transplantation that took place at Mount Sinai in New York City in April this year with 30 fellows from around the world and an international faculty of experts in the field of pediatric transplantation. The IPTA Fellows Symposium provided updates in a broad spectrum of pediatric transplantation, but furthermore, an ideal environment for networking and mentoring. Once again the IPTA Fellows Symposium proved to be very popular amongst trainees, one of them stating that “… the whole meeting was phenomenal and it really helps give "newbies" like us perspective and help in trying to make our mark in the field…”
The Education Committee successfully submitted symposium proposals for the American Transplant Congress in May in Boston, MA, USA, and contributed to the educational content of a Joint IPTA/TTS Pediatric Post Graduate Course at the 26th International Congress of The Transplantation Society in August 2016 in Hong Kong. The Pediatric PG Course reviews listing criteria for children undergoing solid organ transplantation and donor selection, and provides insights on specific aspects of post-transplant care in children.
In the meantime, the Education Committee has already started to organize the educational content of the PG Course planned at the start of the upcoming 9th IPTA Congress to be held in Barcelona, Spain, in May 2017.
ID CARE COMMITTEE UPDATE
Upton Allen, ID CARE Committee Chair
The ID-CARE initiative was formed within IPTA with the idea that one of its main goals would be to serve as the focal point for ID initiatives and to link IPTA with other ID groups where appropriate. The focus is ID Clinical Care, Advocacy, Research and Education. The Committee seeks to engage IPTA members from all disciplines within pediatric organ stem cell transplantation.
The ID CARE Committee has been involved in several initiatives, some of which have been published in Pediatric Transplantation (Curriculum-related documents). In keeping with this approach, the group is currently working on a document that focuses on the evaluation and management of transplant candidates or recipients with recent active infections. A first draft of this document has been completed and submission to Pediatric Transplantation is expected in Fall 2016. The leads are Arnaud L’Huillier, Upton Allen and Michael Green.
The group has also identified other projects which are at varying stages of completion. Among these are the following:
- Status of use of live vaccines after pediatric solid organ. Klara Pofsay-Barbe is leading this initiative. In addition, a survey of current practices has been proposed.
- Pneumocystis prophylaxis strategies across transplant centers. This is being led by Mignon McCulloch and Marian Michaels.
- TB and Transplantation: A Pediatric Perspective. This initiative is led by Mignon McCulloch.
- Yearly Influenza update. This has been proposed as the first in the series of yearly influenza updates be led by Natasha Halasa. This will focus on what is new in influenza molecular epidemiology, antiviral drug resistance, vaccines, treatment and chemoprophylaxis with a focus on immunocompromised patients, notably transplant patients.
Over the upcoming months, the group looks forward to engaging representation from the HSCT group. Collaborations on selected documents or guidelines will also occur. These included, but are not limited to cytomegalovirus (CMV) or Post-transplant lymphoproliferative disorder (PTLD).
PEDIATRIC TRANSPLANTATION UPDATE
Wiley, publisher of Pediatric Transplantation has announced the acquisition of Atypon, one of the world’s leading scientific and scholarly information platform providers.
Wiley is very excited about joining up with our new colleagues at Atypon to bring you the best publishing technology in the industry. Atypon shares our values and focus on the researcher, and working with them is a natural extension of our commitment to providing flexibility to our partners and increasing digital engagement for readers.
Over the next 18 months, we’ll migrate from the platform supporting the Wiley Online Library to Atypon’s Literatum platform. This will bring a number of new benefits to users, including seamless access to content through authenticated article links, improved single-sign-on, editor highlights, article usage metrics, site-wide fully responsive mobile design, minimal-downtime releases, targeted content marketing, article recommendations and e-mail alerting, and more powerful search. This approach will allow us to more rapidly and flexibly respond to the changing needs of the communities we serve.
Wiley will join a diverse array of organizations currently using Atypon’s platform, including societies like the American Chemical Society, Massachusetts Medical Society (publishers of The New England Journal of Medicine), and the American Society of Civil Engineers; publishers such as Elsevier, Sage, and Taylor & Francis, and university presses.
This acquisition is part of our commitment at Wiley to supporting the advancement of scientific and scholarly research and helping authors to reach the widest audience possible and to create impact for their research, investing in the industry’s best technology experience and curating and protecting the version of record.
Contact
+1-514-874-1717
This email address is being protected from spambots. You need JavaScript enabled to view it.
Address
International Pediatric Transplant Association
International Headquarters
505 Boulevard René-Lévesque Ouest
Suite 1401
Montréal, QC, H2Z 1Y7
Canada